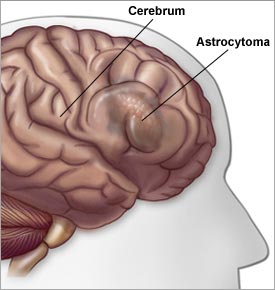
Low Grade Gliomas
Start with this review article (go here or here and see the NCCN site here). The grade and histology are critical in determining the treatment and prognosis for primary brain tumors. Low grade gliomas (grade 1 and 2) are more slow growing and are often treated with surgery.
The role of postOp radiation is somewhat controversial and is discussed below (see CancerNet, and the NCCN guidelines flow chart and the NCCN manuscript,) The treatment of high grade gliomas ( grade 3 anaplastic astrocytoma or grade 4 glioblastoma) are discussed elsewhere.
(Low grade gliomas have a different appearance on MRI or CT compared to glioblastoma see here, here, here, here and here).
Survival tables are noted below. Old age has a negative impact on survival with low grade gliomas. In a large series from the Mayo clinic with patients over 55y the median survival was only 2.7 years (31%/5y and 19%/10y). Other Prognostic factors that affect survival are noted here, age and survival here, grade and survival go here, and the other studies below.
Studies using radiation (go here). Generally if radiation is used the dose is 54Gy in 30 factions as noted in the NCCN guidelines or the RTOG protocol below. The role of radiosurgery in this disease is controversial go here and here
Picture of a low grade glioma before after radiation go here. For more pictures of MRI images go here and here.

