| Background Stereotactic radiosurgery
is the principal alternative to microsurgical resection for acoustic
neuromas
(vestibular schwannomas). The goals of radiosurgery are the long-term
prevention of tumor growth, maintenance of neurologic function, and prevention
of new neurologic deficits. Although acceptable short-term outcomes have
been reported, long-term outcomes have not been well documented. Methods
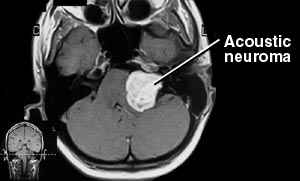
We evaluated 162 consecutive patients who underwent radiosurgery for acoustic
neuromas
between 1987 and 1992 by means of serial imaging tests, clinical evaluations,
and a survey between 5 and 10 years after the procedure. The average dose of
radiation to the tumor margin was 16 Gy, and the mean transverse diameter of
the tumor was 22 mm (range, 8 to 39). Resection had been performed previously
in 42 patients (26 percent); in 13 patients the tumor represented a recurrence
of disease after a previous total resection. Facial function was normal in 76
percent of the patients before radiosurgery, and 20 percent had useful
hearing.
Results The rate of tumor control (with no resection
required) was 98 percent. One hundred tumors (62 percent) became
smaller, 53 (33 percent) remained unchanged in size, and 9 (6 percent) became
slightly larger. Resection was performed in four patients (2 percent) within
four years after radiosurgery. Normal facial function was preserved in 79
percent of the patients after five years (House–Brackmann grade 1), and
normal trigeminal function was preserved in 73 percent. Fifty-one percent of
the patients had no change in hearing ability. No new neurologic deficits
appeared more than 28 months after radiosurgery. An outcomes questionnaire was
returned by 115 patients (77 percent of the 149 patients still living).
Fifty-four of these patients (47 percent) were employed at the time of
radiosurgery, and 37 (69 percent) remained so. Radiosurgery was believed to
have been successful by all 30 patients who had undergone surgery previously
and by 81 (95 percent) of the 85 who had not. Thirty-six of the 115 patients
(31 percent) described at least one complication, which resolved in 56 percent
of those cases.
Conclusions Radiosurgery can provide long-term control of
acoustic
neuromas while preserving neurologic
function.
Radiosurgery Technique
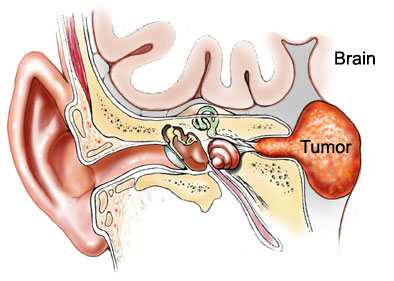
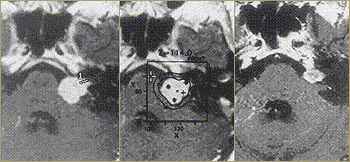
In all patients, stereotactic radiosurgery was performed with a gamma knife. Gamma-knife
radiosurgery provided single-session irradiation of the tumor volume defined by imaging.
The procedure was performed with use of local anesthesia, which was supplemented with
intravenous sedation when necessary. From 1987 through 1990,
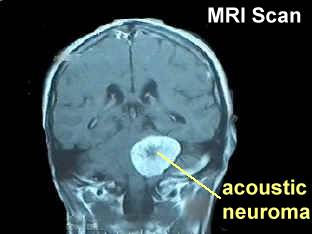
radiosurgery was guided by computed tomographic (CT) imaging. Patients treated in 1991 and 1992 underwent radiosurgery under the guidance of magnetic
resonance imaging (MRI); a prospective comparison study confirmed the accuracy of
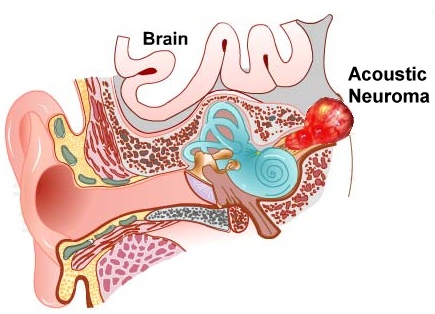
stereotactic targeting based on MRI. Several irradiation isocenters were identified for
use in constructing a radiosurgical plan suitable to the intracanalicular and
extracanalicular components of the tumor. In 126 patients (78 percent) the 50 percent isodose line was used to irradiate the tumor
margin. The image-integrated planning of doses was performed with a computer. For
radiosurgery, the patients lay on the gamma-knife couch and were attached to the
gamma-knife collimator helmet with a stereotactic frame.
Initially, the dose delivered to the tumor margin, 18 to 20 Gy,
was based on experience in a Swedish study. However, the dose to the tumor margin was decreased to an average of 16 to 18 Gy within the first two years and
by 1992 was decreased further, to 14 to 16 Gy. Our serial reevaluation of the
cranial-nerve response prompted small decreases in the dose in order to improve
preservation of cranial-nerve function. The mean dose delivered to the tumor margin in
this series of patients was 16.6 Gy (range, 12 to 20). The mean maximal dose was 32.7 Gy
(range, 24 to 50). The specific doses for individual patients were selected according to
factors that included tumor volume, surgical history, hearing status, facial motor
function, and the patient's wishes. After radiosurgery, all patients received a single
40-mg dose of intravenous methylprednisolone and were discharged from the hospital the
next morning.
Analysis of our results prompted several refinements in our technique. First, we
considered the approximately 30 percent rate of damage to the
facial nerves unacceptable, even though damage was delayed and usually mild.
The initial rate of trigeminal-nerve dysfunction seemed higher than that after resection,
although most resection series did not report this outcome. This finding prompted, in
1989, an average reduction of 2 Gy in the dose of radiation delivered to the tumor
margin. Since the rate of complications did not decline, however, we analyzed our method
of dose planning. We believed that planning doses according to CT findings was an
unsatisfactory approach, since the intracanalicular portion of the tumor could not be well
visualized. However, with MRI, we had a tool that showed the tumor and regional
structures, including cranial-nerve anatomy in great detail. For the first time we could
perform radiosurgery with meticulous targeting, using multiple small isocenters of
irradiation. Advances in high-speed computer workstations facilitated planning. With these
refinements, cranial-nerve morbidity decreased considerably, with
a rate of facial-nerve and trigeminal-nerve side effects that was below 7 percent for
extracanalicular tumors and below 2 percent for intracanalicular tumors. In our
study, 49 patients received radiation to the tumor margin at doses
of up to 15 Gy and had long-term follow-up, and in this group, the high rate of control of
tumor growth was maintained.This finding indicated that the radiation doses
initially thought to be necessary for a tumor response were too high. Radiobiologic
studies showed that the lower dose range causes tumor regression in human xenograft
models. |