|
||
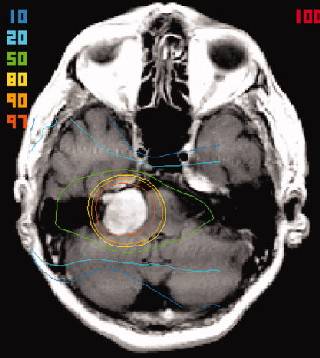
FSRT was well tolerated in all patients. The 5-year actuarial local control rate was 96.2% . Five-year actuarial progression-free survival was 92.8% (95% CI: 84.8%-100.0%). The overall hearing preservation rate was 77.3%. Five of 6 patients with initial cranial nerve V (CNV) numbness remained stable post-FSRT. Two of 3 patients with baseline trigeminal neuralgia improved with the remaining patient stable. All 3 patients with nonsurgically related facial nerve weakness either improved or achieved stability in function. There were no cases of new cranial nerve toxicity post-FSRT. CONCLUSIONS.FSRT for the treatment of AN is safe, effective, and well tolerated. FSRT should thus be considered as an effective alternative treatment modality when compared with microsurgical resection or single fraction stereotactic radiosurgery. Acoustic neuromas (ANs) arise from the Schwann cells of the myelin sheath usually at the vestibular division of the eighth cranial nerve. These benign tumors are typically characterized by slow growth, but may eventually be associated with significant neurologic symptoms related to compression of both involved and adjacent cranial nerves and the brainstem. Ideal treatment for AN should offer a high probability of local control with minimal risks to neural structures. Microsurgery has been the traditional treatment, representing a safe and effective treatment with resultant excellent local control rates ranging from 94% to 99%. Other treatment options for AN include fractionated stereotactic radiotherapy (FSRT) and stereotactic radiosurgery - using both linear accelerator (linac) and gamma knife (GK)-based approaches. FSRT has an advantage in that it combines the target and dose localization characteristics of the radiosurgical system with the radiobiologic advantages of fractionation. It may therefore be associated with a lesser risk of cranial nerve toxicity. Various series of FSRT outcomes in AN have reported 5-year local control rates ranging from 93% to 98% utilizing a variety of fractionation regimens, with a recent series of a 20-year experience with FSRT documenting very long-term efficacy. The FSRT technique involved the use of a relocatable stereotactic Gill-Thomas-Cosman (GTC) frame and multiple non-coplanar converging arcs of 6-MV photon beam, utilizing the Radionics (Burlington, MA) X-Knife radiation treatment planning system with MR-CT image fusion software. The gross tumor volume (GTV) was defined as the area of contrast enhancement on T1-weighted MRI, with the planning target volume (PTV) including a further 1-2 mm safety margin added to account for variance within the treatment planning system. The accuracy of this system has been previously documented as 0.4 mm. The total dose was 50 Gy in 25 daily fractions over 5 weeks, prescribed to the 95% to 100% encompassing isodose. |