|
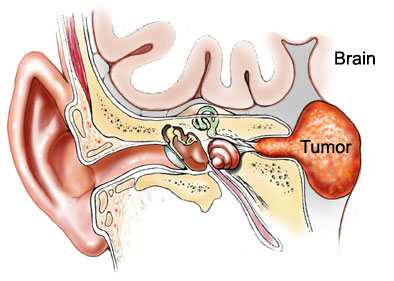
Gamma knife
radiosurgery for vestibular schwannomas: results of hearing
preservation in relation to the cochlear radiation dose.
Timmer FC,
Laryngoscope.
2009 Jun;119(6):1076-81.
OBJECTIVES/HYPOTHESIS: This study was designed
to evaluate hearing preservation after gamma knife radiosurgery (GKRS)
and to determine the relation between hearing preservation and
cochlear radiation dose in patients with a sporadic vestibular
schwannoma (VS). A total of 69 patients were included in the
study. Mean tumor size was 17 mm. Mean marginal dose at the tumor
was 11.0 Gy (range, 9.3 Gy-12.3 Gy), mean maximal dose was 19.7 Gy
(range, 16 Gy-25.5 Gy). Mean maximal dose at the cochlea was 10.27
Gy (range, 3.1 Gy-16.1 Gy), and mean minimal dose at the cochlea was
2.6 Gy (range, 0.9 Gy-7.4 Gy). Hearing was considered to be
preserved (max +1 class, Tokyo classification) in 52 (75%) of 69
patients. However, only 32 patients had class A, B, or C
(serviceable hearing) before GKRS. Within this group, only 13
patients (41%) had a hearing class A, B, or C after GKRS. A
significant relation was found between the maximal cochlear dose and
the difference in PTA before and after GKRS. CONCLUSIONS:
Hearing preservation is
correlated to the maximal radiation dose at the cochlea. The
purpose of developing GKRS techniques was to avoid collateral damage
in healthy tissues. This study emphasizes the need for exact
radiation planning to reduce the cochlear radiation dose if the
hearing is to be preserved.
Stereotactic
radiosurgery for trigeminal schwannoma: tumor control and functional
preservation Clinical article.
Kano H, Niranjan A, Kondziolka
D, Flickinger JC, Dade Lunsford L.
J
Neurosurg. 2009 Mar;110(3):553-8.
The median patient age was 49.5 years (range
15.1-82.5 years). Eleven patients had undergone prior tumor
resection. Two patients had neurofibromatosis Type 2. Lesions were
classified as root type (6 tumors), ganglion type (17 tumors), and
dumbbell type (10 tumors) based on their location. The
median radiosurgery target
volume was 4.2 cm3 (range 0.5-18.0 cm3), and the
median dose to the tumor
margin was 15.0 Gy (range 12-20 Gy).RESULTS: At an average of
6 years (range 7.2-147.9 months), the rate of
progression-free survival (PFS)
at 1, 5, and 10 years after SRS was 97.0, 82.0, and 82.0%,
respectively. Factors associated with improved PFS included female
sex, smaller tumor volume, and a root or ganglion tumor type.
Neurological symptoms or
signs improved in 11 (33.3%) of 33 patients and were unchanged in 19
(57.6%). Three patients (9.1%) had symptomatic disease
progression. Patients who had not undergone a prior tumor resection
were significantly more likely to show improvement in neurological
symptoms or signs.CONCLUSIONS: Stereotactic radiosurgery is an
effective and minimally invasive management option in patients with
residual or newly diagnosed trigeminal schwannomas. Predictors of a
better treatment response included female sex, smaller tumor volume,
root or ganglion tumor type, and the application of SRS as the
primary treatment.
Hearing preservation
after stereotactic radiosurgery for vestibular schwannoma: a
systematic review.
Yang I,
J Clin Neurosci. 2009 Jun;16(6):742-7.
A total of 254 published studies reported
assessable and quantifiable outcome data of patients undergoing
radiosurgery for vestibular schwannomas. American Association of
Otolaryngology-Head and Neck Surgery (AAO-HNS) class A or B and
Gardner-Robertson (GR) classification I or II were defined as having
preserved hearing. A total of 5825 patients (74 articles) met our
inclusion criteria. Practitioners who delivered an
average dose of 12.5 Gy
as the marginal dose reported having a higher hearing preservation
rate (12.5 Gy=59% vs. >12.5
Gy=53%, p=0.0285). Age of the patient was not a significant
prognostic factor for hearing preservation rates (<65 years=58% vs.
>65 years=62%; p=0.4317). The average overall follow-up was 41.2
months. Our data suggest
that an overall hearing preservation rate of about 57% can be
expected after radiosurgical treatment, and patients treated with
12.5 Gy were more likely to have preserved hearing.
Predictors of
hearing preservation after stereotactic radiosurgery for acoustic
neuroma.
Kano H, Kondziolka D, Khan A,
Flickinger JC, Lunsford LD.
J
Neurosurg. 2009 Mar 13.
The authors of this study
evaluated tumor control and hearing preservation as they relate to
tumor volume, imaging characteristics, and nerve and cochlear
radiation dose following stereotactic radiosurgery (SRS) using the
Gamma Knife. Methods Seventy-seven patients with ANs had serviceable
hearing (Gardner-Robertson [GR] Class I or II) and underwent SRS
between 2004 and 2007. This interval reflected more recent
measurements of inner ear dosimetry during the authors' 21-year
experience. The median patient age was 52 years (range 22-82 years).
No patient had undergone any prior treatment for the ANs. The
median tumor volume was 0.75
cm(3) (range 0.07-7.7 cm(3)), and the median radiation dose
to the tumor margin was 12.5
Gy (range 12-13 Gy). At diagnosis, a
greater distance from the
lateral tumor to the end of the internal auditory canal correlated
with better hearing function. Results At a median of 20
months after SRS, no patient required any other additional
treatment. Serviceable
hearing was preserved in 71% of all patients and in
89% (46 patients) of those
with GR Class I hearing. Significant prognostic factors for
maintaining the same GR class included (all pre-SRS) GR Class I
hearing, a speech discrimination score (SDS) >/=80%, a pure tone
average (PTA) < 20 dB, and a patient age < 60 years.
Significant prognostic
factors for serviceable hearing preservation were (all pre-SRS) GR
Class I hearing, an SDS >/=80%, a PTA < 20 dB, a patient age < 60
years, an intracanalicular tumor location, and a tumor volume < 0.75
cm(3). Patients who received a radiation dose of < 4.2 Gy to the
central cochlea had significantly better hearing preservation of the
same GR class. Twelve of 12 patients < 60 years of age who
had received a cochlear dose < 4.2 Gy retained serviceable hearing
at 2 years post-SRS. Conclusions As currently practiced, SRS with
the Gamma Knife preserves serviceable hearing in the majority of
patients. Tumor volume and anatomy relate to the hearing level
before radiosurgery and influence technique. A low radiosurgical
dose to the cochlea enhances hearing preservation.
Vestibular
schwannoma: surgery or gamma knife radiosurgery? A prospective,
nonrandomized study.
Myrseth E, Møller P, Pedersen
PH, Lund-Johansen M.
Neurosurgery. 2009 Apr;64(4):654-61;
OBJECTIVE: To conduct a
prospective, open, nonrandomized study of treatment-associated
morbidity in patients
undergoing microsurgery or gamma knife radiosurgery (GKRS)
for vestibular schwannomas. METHODS: Ninety-one patients with
vestibular schwannomas with a
maximum tumor diameter of 25
mm in the cerebellopontine angle were treated according to a
prospective protocol either by GKRS (63 patients) or open
microsurgery (28 patients) using the suboccipital approach. Primary
end points included hearing function, according to the
Gardner-Robertson scale, and facial nerve function, according to the
House-Brackmann scale at 2 years. Clinical data included a balance
platform test, score for tinnitus and vertigo using a visual analog
scale, and working ability. Patients responded to the
quality-of-life questionnaires Short-Form 36 and Glasgow Benefit
Inventory. RESULTS: Three elderly GKRS patients withdrew; all
remaining patients were followed for 2 years.
Both primary end points were
highly significant in favor of GKRS (P < 0.001). Evidence of
reduced facial nerve
function (House-Brackmann grade 2 or poorer) at 2 years was found in
13 of 28 open microsurgery patients and 1 of 60 GKRS patients.
Thirteen of 28 patients who
underwent surgery had serviceable hearing (Gardner-Robertson grade A
or B) preoperatively, but none had serviceable hearing
postoperatively. Twenty-five of 60 GKRS patients had serviceable
hearing before treatment, and 17 (68%) of them had serviceable
hearing 2 years after treatment. The tinnitus and vertigo
visual analog scale score, as well as balance platform tests, did
not change significantly after treatment, and working status did not
differ between the groups at 2 years.
Quality of life was
significantly better in the GKRS group at 2 years, based on
the Glasgow Benefit Inventory questionnaire. One GKRS patient
required operative treatment within the 2-year study period.
CONCLUSION: This is the second prospective study to demonstrate
better facial nerve and hearing outcomes from GKRS than from open
surgery for small- and medium-sized vestibular schwannomas. |