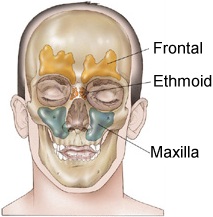
Paranasal
Tumors
(Maxillary and Ethmoid Sinus Cancer)
Anatomy
here, here,
here,
here, here, and here.
Cross section anatomy: here,
here,
here, here
Stage and illustrations
here|
Stage: one, two,
three
MRI of ethmoid cancer
here,
here and
here,
PET scan here
Read the review article , here, here and here
Lymph node risk
here
Survival by histology
here
Survival by stage here
Tumors of the
paranasal sinuses are rare and often asymptomatic until late in the course of their
disease. Although the most common histology for these tumors is squamous cell carcinoma,
multiple pathologies have been reported including sarcomas, lymphomas, adenocarcinomas,
minor salivary gland tumors, and esthesioneuroblastomas. Locoregional control and
incidence of distant metastasis are dependent on both T stage and tumor histology.
However, T stage remains the most reliable predictor of .survival and local regional
control.
A large single institution retrospective analysis included 149 patients with carcinoma of the maxillary sinus treated with radical surgery and postoperative RT (55 to 60 Gy in six weeks). The five-year actuarial overall and cancer-specific survival rates were 36 and 42 percent, respectively. For patients with stage II, III, or IV disease, survival rates were 75, 36, and 11 percent, respectively. The AJCC reports the following 5 year relative survival rates: Stage I = 60.4%, Stage II = 50%, Stage III = 45.9% and Stage IV = 31.1%.
Most of these patients are treated with surgery and postOp radiation( see NCCN guidelines page 1 and page 2 and XRT guidelines.) For a review of postOp radiation go here