PostOperative Radiation
see video
here
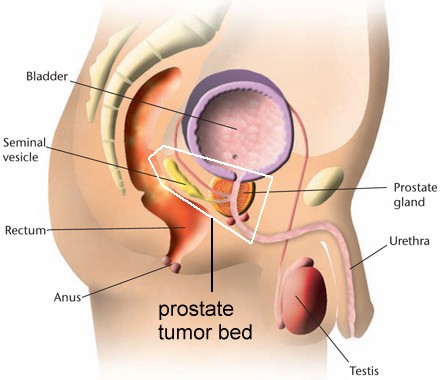
Postoperative radiation (i.e. radiation given to the tumor bed, or the area where the prostate was removed from with a radical prostatectomy) is generally recommended if the pathology report shows that the tumor has spread through the capsule, into the seminal vesicles or has + surgical margins (T3 cancer). Radiation given immediately after recovering from surgery (which may take 6 weeks to 3 months) is called adjuvant or postoperative therapy, and there are three large studies showing the benefit of post operative radiation (go here). Collected data say the best results are when the PSA is the lowest and for every PSA rise of 0.1 the cure rate falls by 4% (go here) and here.
Radiation given to men who have had surgery and later develop a recurrence (usually based on a rising PSA) is called salvage radiation and is discussed separately (go here.)
In general, radiation given after surgery for T3 lesions will improve the local
control and possibly survival as noted (see study
, here ,
here,
here
, here
and study here). Immediate
postOp radiation is particularly beneficial if the surgical margins are
involved (go here).
The proper
dose is being studied (here).
For high risk patients the dose may need to be as high as 72Gy (go
here). The lower the PSA after surgery the better the chance for cure (go
here and here) and the lower
the Gleason the better (here).