RADIATION
THERAPY
The first experience in using radiation
therapy for liver metastases was with
external-beam whole-liver radiotherapy (with
and without systemic or regional
chemotherapy), in which the doses that could
be delivered safely were not high enough to
eradicate metastases. More recently,
technologic advances in radiation treatment
planning allow high-dose radiation therapy
to be delivered conformally around liver
metastases safely, with the potential for
eradication of disease and cure, in
appropriately selected patients. Other types
of radiation have also been used to treat
liver metastases including brachytherapy and
hepatic arterial delivery of
90Y-tagged microspheres. Here, the
experience following whole-liver
irradiation, conformal radiation therapy,
brachytherapy, and hepatic arterial
90Y for treatment of liver metastases
will be reviewed.
Whole-Liver Irradiation
The approach of using whole-liver
irradiation for metastases is limited by the
low tolerance of the whole liver to
irradiation, with doses required to be less
than 30 Gy over 3 weeks to avoid liver
toxicity. Several clinical trials of
whole-liver irradiation for liver metastases
have established the safe whole-liver doses
that can be delivered in a variety of
fractionations. The duration of response and
survival rates tend to be short. In
contrast, low-dose whole-liver irradiation
can produce palliation of painful liver
metastases in the majority of cases. In an
attempt to improve on the poor outcomes
following whole-liver irradiation alone,
whole-liver irradiation has been combined
with systemic or regional chemotherapy. The
most widely used drugs in this effort have
been the fluoropyrimidines because of their
activity against CRC and their
radiation-sensitizing properties . In
general, the response rates and survival
rates following combined-modality therapy
seem to be superior to those obtained
following whole-liver irradiation alone.
Selection bias may be at least partially
responsible for this effect. A recent study
demonstrated that whole-liver radiation (20
Gy in 10 fractions) does not improve the
efficacy of 5-FU for patients who have
diffuse liver metastases.
Conformal Radiation Therapy
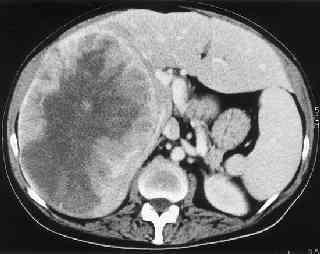
Technical advances in
liver cancer imaging, radiation planning,
methods to account for breathing motion
during radiation delivery and image guidance
at the time of radiation delivery have made
it possible to deliver high-dose radiation
safely to focal liver metastases, while
sparing irradiation of the uninvolved liver,
using a variety of radiation fractionation
schedules.In most studies, higher doses of
radiation have been associated with more
durable local control rates than lower
doses, regardless of the fractionation
schedule. Since the late 1980s at the
University of Michigan, a series of phase
I/II trials for patients with unresectable
intrahepatic cancer have investigated
dose-escalated conformal radiation therapy
delivered concurrently with hepatic arterial
chemotherapy (predominantly floxuridine [0.2
mg/kg/day]). In one of the first studies,
the objective response rate of 22 patients
with unresectable CRC liver metastases,
treated with as much as 72.6 Gy at 1.5 Gy
twice daily, was 50% (2 complete remission,
9 partial response, 11 stable disease),with
a median survival of 20 months. Similar
results were obtained in subsequent studies,
including the most recent study in which the
prescription dose was individualized based
on the volume of liver irradiated and risk
of toxicity, allowing higher doses (as much
as 90 Gy at 1.5 Gy twice daily) to be
delivered safely to more patients. The
median survival of 47 patients with liver
metastases (median diameter ∼10 cm) treated
on this study was 17.2 months.
Stereotactic body
radiation therapy (SBRT), referring to a
limited number of high-dose fractions
delivered very conformally to targets, using
biologic doses of radiation higher than
those used in standard fractionation, has
also been used to treat liver metastases.
Safety of 1- to 10-fraction SBRT has been
described in several retrospective series
and more recently confirmed in prospective
dose escalation studies. Blomgren and
colleagues from Sweden first reported a
response rate of 43% for 14 liver metastases
treated with 20 to 45 Gy in one to four
fractions, with a prolonged time to maximal
response (e.g., maximal response at 16
months for a 13-cm liver metastases). No
liver toxicity was seen in patients with
metastases, but hemorrhagic gastritis was
seen in one patient. In an update in 1998,
the local control rate was 95% with a mean
survival of 17.8 months for 21 liver
metastases.SBRT (20 Gy × 2 or 15 Gy × 3) has
also been used safely in patients with
recurrent liver metastases following hepatic
resection for CRC metastases, with no
serious toxicity and local control 13 to 101
months following surgery. A prospective
study of escalated single-fraction SBRT (14
Gy to 26 Gy) did not find a maximal
tolerated dose in 60 liver tumors (56
metastases) with a median tumor size of 10
mL (1–132 mL) and found an actuarial local
control rate of 81% at 18 months following
SBRT.
SBRT delivered in three
fractions (37.5 Gy total) has also been
reported to be safe in small liver
metastases, with 2-year local control and
survival rates of 61% and 41%, respectively.
A North American prospective
study confirmed the safety of three-fraction
SBRT in 18 patients with 25 tumors of
maximal diameter 6 cm.
A Canadian prospective study
has shown the feasibility of delivering
six-fraction SBRT using an individualized
dose allocation approach as first described
by the Michigan group, for liver cancers
ranging from 3 to 3,000 mL.
More recently,
outcomes following SBRT for 174 liver
metastases from colorectal, pancreatic,
breast, and lung cancer in 69 patients were
reported. The median dose delivered was 48
Gy (range 30–55 Gy) at 2 to 6 Gy per
fraction. The local control was 76% and 57%
at 10 and 20 months, respectively, with an
overall medial survival of 14.5 months. No
grade 3 toxicity was reported. Based on this
experience, 10-fraction SBRT is being
studied in a Radiation Therapy Oncology
Group study that is now open.
Liver Tolerance to
Irradiation
In the early 1960s it
was found that doses greater than 30 Gy at 2
Gy per fraction to the whole liver led to an
unacceptable risk of liver toxicity. Eight
fractions of 2.25 Gy to the whole liver was
found to be safe, but a small increase in
fraction size to 3.5 Gy was reported in 1973
to be associated with an unacceptable rate
of liver toxicity (8 of 25 patients). The
tolerance of the liver to whole-organ
irradiation does not seem to be
substantially altered by the concomitant use
of fluoropyrimidines. In contrast,
whole-liver irradiation in combination with
alkylating agents or mitomycin C is
associated with an increased risk of liver
toxicity. Liver toxicity following
irradiation has historically been referred
to as “radiation hepatitis” and more
recently termed “radiation-induced liver
disease" (RILD), because there is no
evidence of hepatitis on pathologic
examination. This complication is a clinical
syndrome consisting of anicteric ascites and
painful hepatomegaly, occurring in the
absence of disease progression, usually
within 3 months following a course of
radiation therapy. Laboratory evaluation
demonstrates a marked elevation of alkaline
phosphatase out of proportion to the modest
increases in the transaminases. Although the
majority of patients recover from RILD, it
may progress to liver failure and death. The
pathophysiology of RILD is not well
understood. Pathologically, venoocclusive
disease, similar to that seen following bone
marrow translation, is seen.
Partial liver
radiation therapy was first reported in 1965
by Ingold and associates, who safely
delivered as much as 55 Gy to parts of the
liver. Others confirmed that high-dose
radiation therapy could be delivered safely,
as long as a substantial portion of the
normal liver was spared. Conformal radiation
planning permits portions of the liver to be
treated with doses of radiation far higher
than what the entire liver can tolerate so
long as a sufficient volume of uninvolved
liver can be spared from irradiation,
similar to how a surgeon can resect a
substantial fraction of the liver if the
remaining liver is functional. Conformal
radiation treatment planning allows the
fraction of uninvolved liver irradiated to
be quantified. Theoretical models have been
proposed to estimate the volume dependence
of normal tissue tolerance—referred to as
normal tissue complication probability (NTCP)
models.
Such an NTCP model has been used
to describe the partial liver tolerance of
203 patients treated with conformal
hyperfractionated radiation therapy and
hepatic arterial floxuridine (17 of whom
developed RILD). This analysis found that
that mean liver dose can provide an estimate
of the risk of RILD occurring, with a 5%
risk of toxicity following 32 Gy and 37 Gy
in 1.5 Gy twice daily for patients with
primary liver cancer and metastases,
respectively.
The partial volume
tolerance of the liver to hypofractionation
or SBRT has not been well established,
partially in that the majority of clinical
SBRT experience has not required large liver
volumes to be irradiated. Guidelines used in
SBRT planning include sparing of 30% and 50%
of the liver from 12 Gy and 7 Gy,
respectively, for three- and one-fraction
SBRT), and ensuring that at least 700 mL of
uninvolved liver receives less than 15 Gy in
three fractions. Dawson and coworkers have
shown the feasibility of using an NTCP model
for allocation of six-fraction SBRT in over
80 patients, with a wide range of liver
volumes irradiated.
The safe delivery of
high-dose
90Y to small volumes seems consistent
with the partial volume estimates from
conformal radiation and SBRT series, where
the upper limit on the dose of radiation
that can be delivered to an effective liver
volume irradiated of 20% or less has not
been established. The lack of a validated
dose distribution in
90Y treatment makes partial liver
tolerance analysis challenging for
90Y therapy.
Extrapolation of NTCP
models and partial liver tolerances to
different centers must be done with caution,
because the results may not be valid for
different patient populations treated with
different treatments. The partial liver
tolerance to irradiation, especially in
diseased livers and following SBRT and
90Y, should be measured and validated
in prospective studies.
FUTURE
DIRECTIONS
Although it is
becoming established that radiation therapy,
delivered using conformal radiotherapy, SBRT,
brachytherapy, or
90Y microspheres, can be used safely
to treat liver metastases with the potential
for sustained local control, recurrences
outside the irradiated volume are not
infrequent, providing a rationale for
combining radiation therapy with other
therapies. One possibility would be to
combine radiation therapy with repeated
cycles of modern hepatic arterial and
systemic chemotherapy. More potent radiation
tumor sensitizers could also be explored.
Studies of targeted therapies combined with
radiotherapy should be considered, given the
radiation sensitization properties of many
targeted agents and survival gains observed
following the combination of radiation and
targeted agents in other clinical
sites.Conversely, normal-tissue radiation
protectors, as well as more technologic
advances, may allow higher doses to be
delivered to more tumors safely. For
instance, the free-radical scavenger
amifostine protects the normal liver (but
not tumor) from radiation in preclinical
studies. It is hoped that these approaches
will permit a greater fraction of patients
to benefit from high-dose therapy and will
increase local control in patients with
localized unresectable intrahepatic cancers.
|