Escalated focal liver radiation and concurrent hepatic
artery fluorodeoxyuridine for unresectable intrahepatic malignancies.
Dawson LA, .J Clin Oncol. 2000 Jun;18(11):2210-8.
Departments of Radiation Oncology, Internal Medicine, and Pharmacology, University of
Michigan, Ann Arbor
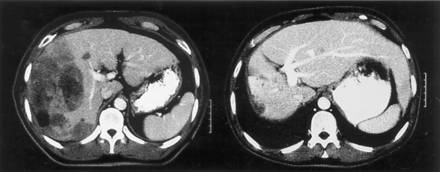
PURPOSE: To evaluate the response, time to progression, survival, and impact of radiation
(RT) dose on survival in patients with intrahepatic malignancies treated on a phase I
trial of escalated focal liver RT. PATIENTS AND METHODS: From April 1996 to January 1998,
43 patients with unresectable intrahepatic hepatobiliary cancer (HB; 27 patients) and
colorectal liver metastases (LM; 16 patients) were treated with high-dose
conformal RT. The median tumor size was 10 x 10 x 8 cm. The median
RT dose was 58.5 Gy (range, 28.5 to 90 Gy), 1.5 Gy twice daily, with concurrent
continuous-infusion hepatic arterial fluorodeoxyuridine (0.2 mg/kg/d) during the first 4
weeks of RT. RESULTS: The response rate in 25 assessable patients was 68% (16 partial and
one complete response). With a median potential follow-up period of 26.5 months, the
median times to progression for all tumors, LM, and HB were 6, 8, and 3 months,
respectively. The median survival times of all patients, patients with LM, and patients
with HB were 16, 18, and 11 months, respectively. On multivariate analyses, escalated RT
dose was independently associated with improved progression-free and overall survival. The
median survival of patients treated with 70 Gy or more has not
yet been reached (16.4+ months), compared with 11.6 months in patients treated with lower
RT doses (P =.0003). CONCLUSION: The excellent response rate, prolonged
intrahepatic control, and improved survival in patients treated with RT doses of 70 Gy or
more motivate continuation of dose-escalation studies for patients with intrahepatic
malignancies.The role of radiotherapy in the treatment of liver
metastases.
Dawson LA, Lawrence TS. Cancer J. 2004 Mar-Apr;10(2):139-44.
Department of Radiation Oncology, Princess Margaret Hospital, University of Toronto,
Toronto, Ontario, Canada. laura.dawson@rmp.uhn.on.ca
Radiotherapy has historically played a minor role in the treatment of patients with
unresectable liver metastases from colorectal cancer and other malignancies. This can be
attributed chiefly to the low tolerance of the whole liver to radiation. High-precision radiotherapy planning techniques have allowed much
higher doses of radiation to be delivered safely to focal liver metastases, while sparing
most of the normal liver. When combined with
hepatic arterial fluorodeoxyuridine, high-dose focal liver radiotherapy is associated with
excellent response rates, local control, and survival in patients with unresectable liver
metastases from colorectal cancer. Radiotherapy, with and without concurrent systemic
chemotherapy, has also been used with encouraging outcomes for patients with liver
metastases from colorectal cancer and other cancers. There appears to be a radiation dose
response for liver metastases; tumors treated with doses of 70 Gy
or greater are likelier to have durable local control. Advancements in tumor
imaging, in radiotherapy techniques that will allow the safe delivery of higher doses of
radiation, and in novel tumor radiation sensitizers and normal tissue radioprotectors
should substantially improve the outcome of patients with unresectable liver metastases
treated with radiotherapy.
Radiotherapy of liver malignancies. From whole liver irradiation to
stereotactic hypofractionated radiotherapy.
Greco C,Tumori. 2004 Jan-Feb;90(1):73-9.
Division of Radiation Oncology, European Institute of Oncology, Milan, Italy.
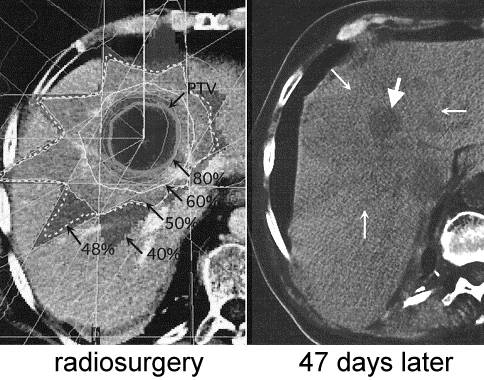
AIMS AND BACKGROUND: Until recently radiotherapy of hepatic malignancies has played a
limited role due to the well-known limited radiotolerance of the liver. The aim of this
paper is to review the available data on the risk of radiation-induced liver disease
(RILD) and to define the modern role of radiotherapy in the management of patients with
metastatic or primary liver malignancies. METHODS: The advent of three-dimensional
conformal treatment planning with dose-volume histogram analysis has made the study of
partial liver irradiation possible. Limited portions of the liver may withstand high doses
of radiation with minimal risk of RILD. Patients with solitary unresectable liver tumors
may be treated with high-dose radiotherapy with curative intent. Recently, the feasibility
of stereotactically guided treatment techniques with a single fraction or few treatment
sessions has been explored in numerous institutions. RESULTS: The radiation
tolerance of the whole liver found by several investigations is in the order of
approximately 30 Gy, which seriously restricts its clinical application. The
role of whole liver irradiation therefore appears of limited benefit in the palliation of
patients with multiple liver metastases. The use of three-dimensional
conformal techniques has made partial liver irradiation possible to doses in the 70-80 Gy range
with conventional fractionation. At least two published series have reported improved
local control and survival rates with dose escalation with three-dimensional conformal
radiotherapy in patients with unresectable liver metastases. Similar outcomes have been
recently reported with single dose (or hypofractionated) stereotactic radiotherapy both in
metastatic and primary hepatic malignancies with minimal morbidity. Accurate target
delineation and treatment reproducibility are the key to the success of this novel
treatment approach, and specific treatment planning techniques and patient setup
procedures must be developed to implement it. CONCLUSIONS: Stereotactic high-dose
radiotherapy is technically feasible for the treatment of inoperable liver malignancies,
with the potential of high local control and low morbidity. Definitive evidence on the
clinical advantages of this technique over other more established treatments can only be
gathered from well-designed clinical studies.
Treatment of intrahepatic cancers with radiation doses based on a
normal tissue complication probability model.
McGinn CJ, J Clin Oncol. 1998 Jun;16(6):2246-52.
Department of Radiation Oncology, University of Michigan Medical School, Ann Arbor
48109-0010, USA. mcginn@umich.edu
PURPOSE: To attempt to safely escalate the dose of radiation for patients with
intrahepatic cancer, we designed a protocol in which each patient received the maximum
possible dose while being subjected to a 10% risk of radiation-induced liver disease
(RILD, or radiation hepatitis) based on a normal tissue complication probability (NTCP)
model. We had two hypotheses: H1; with this approach, we could safely deliver higher doses
of radiation than we would have prescribed based on our previous protocol, and H2; the
model would predict the observed complication probability (10%). PATIENTS AND METHODS:
Patients with either primary hepatobiliary cancer or colorectal cancer metastatic to the
liver and normal liver function were eligible. We used an NTCP model with parameters
calculated from our previous patient data to prescribe a dose that subjected each patient
to a 10% complication risk within the model. Treatment was delivered with concurrent
hepatic arterial fluorodeoxyuridine (HA FUdR). Patients were evaluated for RILD 2 and 4
months after the completion of treatment. RESULTS: Twenty-one patients completed treatment
and were followed up for at least 3 months. The mean dose
delivered by the current protocol was 56.6 +/- 2.31 Gy (range, 40.5 to 81 Gy).
This dose was significantly greater than the dose that would have been prescribed by the
previous protocol (46.0 +/- 1.65 Gy; range, 33 to 66 Gy; P < .01). These data are
consistent with H1. One of 21 patients developed RILD. The complication
rate of 4.8% (95% confidence interval, 0% to 23.8%) did not differ
significantly from the predicted 8.8% NTCP (based on dose delivered) and excluded a 25%
true incidence rate (P < .05). This finding supports H2. CONCLUSION: Our results
suggest that an NTCP model can be used prospectively to safely deliver far greater doses
of radiation for patients with intrahepatic cancer than with previous approaches. Although
the observed complication probability is within the confidence intervals of our model, it
is possible that this model overestimates the risk of complication and that further dose
escalation will be possible. Additional follow-up and accrual will be required to
determine if these higher doses produce further improvements in response and survival.
Combined liver radiation and chemotherapy for palliation of hepatic
metastases from colorectal cancer.
Mohiuddin M, Chen E, Ahmad N. J Clin Oncol. 1996 Mar;14(3):722-8.
Department of Radiation Medicine, University of Kentucky, Lexington, USA.
PURPOSE: To report the effects of boost dose radiation on palliation, survival, and
toxicity in patients undergoing palliative treatment for hepatic metastases from
colorectal cancers and to assess the potential benefits of higher doses of radiation to
partial liver volumes. MATERIALS AND METHODS: Forty-five patients with hepatic metastases
from colorectal cancers were treated with a course of palliative irradiation. Eligible
patients included those with radiographically or histologically proven liver metastases.
All patients but one received chemotherapy, either pretreatment (one patient) and/or
concurrently with radiation (43 patients) via intravenous or hepatic intraarterial
infusion. Patients were divided into two groups based on whether or not boost radiation
was given. Thirty-three of the 45 patients (group 1) received
whole-liver irradiation at doses that ranged from 8 to 31 Gy at 2.0 to 3.0 Gy per fraction
(median dose, 21 Gy). The remaining 12 patients (group
2) received liver irradiation to 20 to 30 Gy followed by a boost dose to the area of
dominant disease for a total dose of 33 to 60 Gy. The extent of liver
involvement was similar between the two groups. Palliation, overall survival, and toxicity
were analyzed with respect to radiation dose. RESULTS: There was no
increase in acute effects observed in treating partial liver volumes to higher
doses in conjunction with systemic chemotherapy. No cases of radiation-induced hepatitis
or nephritis were documented. Hematologic toxicity (> or = grade 3) was observed in
four patients with thrombocytopenia, three with leukopenia, and two with anemia. Pain was relieved in 71% and hepatomegaly in 59% of group 1 patients,
as compared with 100% and 89%, respectively, of group 2 patients. Other
symptoms such as nausea, fever, fatigue, and jaundice were palliated in 35% of group 1 and
90% of group 2 patients. The median survival time for group 1
patients was 4 months (range, 1 week to 26 months), which is consistent with that reported
in the literature. The median survival time for group 2 patients was 14 months
(range, 2 to 32 months) (P=.01). CONCLUSION: Standard hepatic irradiation followed by
boost radiation to partial liver volumes in combination with chemotherapy is well
tolerated without significant acute/late morbidity. Higher radiation doses to partial
liver volumes offers improved palliative benefit and may prolong survival without an
increase in morbidity. |