Int J Cancer 1999 Dec 10;83(6):823-7
Radiotherapy for stages I and IIA/B testicular seminoma.
Bamberg M, Schmidberger H, Meisner C, Classen J, Souchon
R, Weinknecht S, Schorcht J, Walter F, Engenhart-Cabillic R, Schulz U, Born H, Flink M
Department of Radiotherapy, University of Tuebingen,
Germany.
Radiotherapy is generally accepted as a standard treatment
for early-stage testicular seminoma. Relapse rates of 2% to 5% in
clinical stage I and 10% to 20% in stage IIA/B (according to the Royal Marsden
classification) can be achieved. Disease-specific survival reaches 100%. With such
excellent cure rates, treatment-related side effects gain particular importance.
Therefore, a prospective multicenter trial was initiated for radiotherapy of testicular
seminoma with limited treatment portals and low total doses of irradiation. In clinical
stage I, 483 patients were treated with 26 Gy to the para-aortic region only. In stage
IIA, 42 patients and, in stage IIB, 18 patients received irradiation to the para-aortic
and high iliac lymph nodes with 30 and 36 Gy, respectively. With a median time to
follow-up of 55 months for stage I and 55.5 months for stage IIA/B, there were 18 (3.7%)
and 4 (6.7%) cases of relapse in both treatment groups. Disease-specific survival was
99.6% in stage I and 100% in stage IIA/B. Acute toxicity was dominated by moderate
gastro-intestinal side effects. No major late toxicity has been observed to date. Limited volume pure para-aortic treatment for stage I and para-aortic/high
iliac irradiation for stage IIA/B with 26, 30 and 36 Gy, respectively, yields excellent
cure rates with only moderate acute toxicity and is therefore recommended as standard
treatment.
Int J Radiat Oncol Biol Phys 1998 Sep 1;42(2):313-7
Postoperative radiotherapy for Stage I/II seminoma:
results for 212 patients.
Bauman GS, Venkatesan VM, Ago CT, Radwan JS, Dar AR,
Winquist EW
Department of Radiation, London Regional Cancer Centre,
Ontario, Canada.
Between 1950 and 1995, 212 patients seen at the London
Regional Cancer Centre received adjuvant radiotherapy following orchiectomy for Stage I
(169) and II (43) seminoma. Median follow-up for the group was 7.5 years. RESULTS: Progression free, cause specific, and overall survival were 95%, 98%, and
95% at 5 years, and 94%, 98%, and 94% at 10 years respectively. An increased risk
of failure was noted among patients with bulky Stage II disease. No other prognostic
factors for relapse were identified. Late toxicity was uncommon with only 12/212 (6%)
developing any late GI toxicity potentially attributable to radiotherapy. The incidence of second malignancies (excluding second testicular tumors)
was 6/212 (actuarial:1%, 1%, 6% at 5,10,15 years respectively). There was a
trend toward increased acute complications for patients treated with larger volumes of
radiation. Post-operative radiotherapy remains a safe and efficacious adjuvant treatment
for Stage I and early Stage II seminoma.
Clin Oncol (R Coll Radiol) 1998;10(4):237-41
The management and clinical course of testicular seminoma:
15 years' experience at a single institution.
Coleman JM, Coleman RE, Turner AR, Radstone CR, Champion
AE
Weston Park Hospital NHS Trust, Sheffield, UK.
Testicular seminoma is one of the most curable solid
neoplasms, with 5-year survival rates in excess of 90%. However, controversy persists
around its optimum management, particularly for Stage I disease. The outcome of 314
patients with testicular seminoma who were treated at a single institution is reported. A
comparison of adjuvant radiotherapy and surveillance for Stage I is presented, and the
possible prognostic influence of an elevated serum beta-human chorionic gonadotrophin
(beta hCG) is assessed. The 5-year disease-free survival for all stages of presentation
was 95.5%. There were more relapses in Stage I patients undergoing
surveillance (14/94, 15%) than postorchidectomy radiotherapy (6/144, 4%; P = < 0.05).
However, survival was identical irrespective of treatment policy, with no disease-related
deaths in either group of Stage I patients. There were eight tumour-related deaths from
advanced disease and 14 deaths from non-tumour causes. Three were due to cardiorespiratory
disease, four to an unrelated second malignancy, two from infection and one from suicide;
in four patients, the cause was unknown. Preoperative beta hCG was elevated in 29 (18%) of
Stage I patients and in 24 (62%) of those presenting with Stage II disease. Patients were
more likely to have advanced disease (> or = Stage II) if beta hCG was elevated (P <
0.001). Neither disease-free nor overall survival were influenced by the preoperative
level of beta hCG. Surveillance appears to be a safe alternative to postorchidectomy
radiotherapy for Stage I disease, provided the patient is prepared for intensive long term
follow-up. An increased risk of relapse, but not of tumour death, can be expected and
unnecessary treatments avoided.
Strahlenther Onkol 1996 Apr;172(4):186-92
Results of radiotherapy for 230 patients with stage I-II
seminomas.
Hultenschmidt B, Budach V, Genters K, Sack H
Department of Radiooncology, University of Essen.
From 1978 to 1992, 230 male patients with the diagnosis of
pure seminoma of the testis were treated by postoperative radiotherapy at the University
of Essen. According to the Royal Marsden Staging System, 188 patients were presenting with
stage I disease, 24 with stage IIA, 13 with stage IIB and 5 with stage IIC disease. All
patients received irradiation to the paraaortic lymph nodes (median
dose: 36 Gy). In 154 patients the ipsilateral iliac lymph
nodes were additionally irradiated with or without inguinal lymph nodes and in 66
patients the contralateral pelvic nodes were included. Since
1987, the total dose was reduced to 26 Gy for microscopic disease. A
mediastinal irradiation (median dose: 30 Gy) was performed in 22 patients. Eight patients
with stage IIB and IIC disease were additionally treated with chemotherapy. RESULTS: Overall actuarial survival (Kaplan-Meier method) for all patients was
97.8% at 5 years and 96.5% at 10 years. Ten-year survival corrected for intercurrent
mortality (n = 8) was 100%. In 5 patients recurrent disease (n = 5) was observed,
in 6 patients seminoma occurred in the contralateral testis. For stage I seminoma the
disease-free survival was 96.8%. For the whole group of stage II seminoma the DFS was
88.1%, for stage IIA 91.7% and for stage IIB 76.9%. In stage IIC no recurrences occurred.
In general, the radiation therapy was well tolerated with minor side effects only.
CONCLUSIONS: Postoperative radiotherapy for seminoma stage I, IIA and IIB alone offers
excellent control and survival rates with tolerable side effects.
J Clin Oncol 1999 Apr;17(4):1146
Optimal planning target volume for stage I testicular
seminoma: A Medical Research Council randomized trial. Medical Research Council Testicular
Tumor Working Group.
Fossa SD, Horwich A, Russell JM, Roberts JT, Cullen MH,
Hodson NJ, Jones WG, Yosef H, Duchesne GM, Owen JR, Grosch EJ, Chetiyawardana AD, Reed NS,
Widmer B, Stenning SP
Norwegian Radium Hospital, Oslo, Norway.
s.d.fossa@klinmed.u10.no
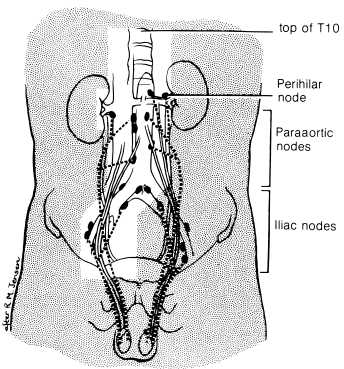
PURPOSE: To compare relapse rates and toxicity associated
with para-aortic (PA) strip or PA and ipsilateral iliac lymph node irradiation (dogleg
[DL] field) (30 Gy/15 fractions/3 weeks) for stage I
testicular seminoma. PATIENTS AND METHODS: Between July 1989 and May 1993, 478 men with
testicular seminoma stage I (T1 to T3; no ipsilateral inguinoscrotal operation before
orchiectomy) were randomized (PA, 236 patients; DL, 242 patients). RESULTS: Median
follow-up time is 4.5 years. Eighteen relapses, nine in each treatment group, have
occurred 4 to 35 months after radiotherapy; among these, four were pelvic relapses, all
occurring after PA radiotherapy. However, the 95% confidence interval (CI) for the
difference in pelvic relapse rates excludes differences of more than 4%. The 3-year relapse-free survival was 96% (95% CI, 94% to 99%) after PA
radiotherapy and 96.6% (95% CI, 94% to 99%) after DL (difference, 0.6%; 95% confidence
limits, -3.4%, +4.6%). One patient (PA field) has died from seminoma. Survival at 3
years was 99.3% for PA and 100% for DL radiotherapy. Acute toxicity (nausea, vomiting,
leukopenia) was less frequent and less pronounced in patients in the PA arm. Within the
first 18 months of follow-up, the sperm counts were significantly higher after PA than
after DL irradiation. CONCLUSION: In patients with testicular seminoma stage I (T1 to T3)
and with undisturbed lymphatic drainage, adjuvant radiotherapy confined to the PA lymph
nodes is associated with reduced hematologic, gastrointestinal, and gonadal toxicity, but
with a higher risk of pelvic recurrence, compared with DL radiotherapy. The recurrence
rate is low with either treatment. PA radiotherapy is recommended as standard treatment in
these patients.
Semin Oncol 1998 Apr;25(2):160-73
Early stage and advanced seminoma: role of radiation
therapy, surgery, and chemotherapy.
Gospodarwicz MK, Sturgeon JF, Jewett MA
Department of Radiation Oncology, Princess Margaret
Hospital and University of Toronto, Ontario, Canada.
Testicular seminoma is an uncommon tumor that accounts for
approximately 50% of all germ cell testicular tumors. The vast majority of patients
present with early-stage disease and almost all patients are cured of their disease.
Management is based on disease extent with patients with stage I seminoma having numerous
treatment options, varying from surveillance to adjuvant retroperitoneal radiation therapy
and prophylactic adjuvant single-agent chemotherapy. Only 20% of patients present with
more advanced disease; the majority of those have stage II disease with retroperitoneal
lymph node involvement. The standard management is retroperitoneal radiation therapy with
chemotherapy being used for patients with bulky disease. Systemic chemotherapy with
cisplatin alone or etoposide and cisplatin is the standard approach to advanced and
metastatic disease with cure rates approaching 85% to 90%.
Int J Urol 1998 Jul;5(4):357-60
Long-term results of adjuvant irradiation or surveillance
in stage I testicular seminoma.
Miki T, Nonomura N, Saiki S, Kotake T
Department of Urology, Osaka University Medical School,
Suita, Japan.
Twenty-seven patients who underwent prophylactic radiation
therapy (RT group) and 41 patients followed only by surveillance (S group) after high
orchiectomy were evaluated. Their follow-up consisted of frequent clinical examinations,
abdominal CT scans, chest x-rays and serum tumor markers. RESULTS: In
the RT group, with a median follow-up period of 15 years, 1 patient (3.6%) had a
recurrence in the lung at 4 months after orchiectomy and died, but the remaining 26 are
alive with no evidence of disease (NED). In the S group, with a median follow-up period of
7.3 years, 5 (12.2%) relapsed in the retroperitoneal lymph nodes, but all are alive
with NED following chemotherapy. The remaining 36 are all alive without recurrence
(follow-up period, 38 to 132 months). Although the relapse rate in the S group was
relatively higher than in the RT group, there was no significant difference between the 2
groups. CONCLUSION: If a frequent follow-up protocol is administered and followed by the
patient, surveillance alone may be a recommended management for stage I testicular
seminoma.
Arch Esp Urol 2000 Jul-Aug;53(6):505-16
[Radiotherapy for the treatment of testicular seminomas].
Sancho Pardo G, Gomez de Segura G
Servicio de Oncologia Radioterapica, Hospital de la Santa
Cruz y San Pablo, Barcelona, Espana.
OBJECTIVE: Conventional treatment of testicular seminoma
has been orchiectomy followed by adjuvant lymph node irradiation. Over the last 10 years
the role of postoperative elective radiotherapy has been questioned. This paper reviews
the role of radiotherapy in the treatment of seminoma of the testis. METHODS: The
literature is reviewed with special reference to the results achieved in the treatment of
testicular seminoma with and without radiotherapy. The advantages and disadvantages of
postoperative radiotherapy, the techniques and dose administered are discussed.
RESULTS/CONCLUSIONS: The results obtained with radiotherapy
postorchidectomy in stage I seminoma of the testis are excellent, with a disease free
survival of 95%-100%. The use of more limited fields of irradiation and lower dose
has reduced the radiation-induced toxicity. Currently, many centers have opted for
clinical surveillance after orchiectomy. Their experience have permitted identification of
the risk factors and there have been attempts to identify the group of patients that
benefit from adjuvant therapy. The low incidence of stage II tumors has not permitted
performing randomized studies to determine the benefits of adjuvant therapy and its
comparison with chemotherapy. Consolidation radiotherapy for bulky stage II and stage III
and IV tumors continues to be a controversy, although its potential value in carefully
selected patients is recognized.
Int J Radiat Oncol Biol Phys 1998 Jan 15;40(2):455-9
Para-aortic irradiation only appears to be adequate
treatment for patients with Stage I seminoma of the testis.
Sultanem K, Souhami L, Benk V, Bahary JP, Roman T,
Shenouda G, Freeman C
Department of Oncology, McGill University, Montreal,
Quebec, Canada.
PURPOSE: Results of treatment of patients with Stage I
seminoma with orchiectomy and radiotherapy are excellent. Even
without adjuvant radiotherapy, the relapse rate is only 15-20%; most of the
patients fail in the retroperitoneum, with rare failures observed in the pelvis (0.5-2%).
In 1991, we began a prospective study evaluating para-aortic lymph node radiation as the
only adjuvant treatment for such patients. This paper reports our preliminary results.
MATERIALS & METHODS: Between March 1991 and January 1996, 35 patients with
histologically proven Stage I seminoma were entered in the study. Median age was 37.9
years (range: 27-65 years). A radical inguinal orchiectomy was performed in all patients.
Staging workup consisted of a chest X-ray; B-HCG, alpha-fetoprotein, and CT scan of the
abdomen and pelvis in all patients. Lymphangiogram was done in 23 (66%) of 35 patients for
further evaluation of the retroperitoneal lymph nodes. Radiotherapy consisted of treatment
to the para-aortic region only. Parallel opposed fields extending from the top of T11 to
the bottom of L5 were used. The median field size was 8.7 x 21.8 cm (range: 7-11 x 18-26
cm). The median total dose, prescribed at midpoint, was 25 Gy given
in 15 daily fractions of 1.66 Gy. Follow-up was performed every 3 months for the
first year, every 4-5 months for the second and third years, and every 6 months
thereafter. Chest X-ray, tumor markers, and CT scan of the pelvis were performed routinely
as part of the follow-up investigation. RESULTS: At a median follow-up of 39.7 months
(range: 16-74 months), 34 (97.1%) of 35 patients are alive with no
evidence of disease for an overall actuarial survival rate of 97.1% at 5 years and a
cause-specific actuarial survival rate of 100%. Treatment morbidity was limited to
Grade I-II acute side effects in 18 (51.4%) of 35 patients. No late side effects were
seen. CONCLUSION: From our preliminary results, adjuvant radiation treatment limited to
the para-aortic lymph node region, without ipsilateral pelvic irradiation, appears to be
adequate treatment for Stage I seminoma. Such an approach in our patients resulted in
minimal toxicity and excellent disease-free survival.
Long-term outcome of postorchiectomy
radiation therapy for stage I and II testicular seminoma.
Akimoto T, Anticancer Res. 1997 Sep-Oct;17(5B):3781-5.
Department of Radiology and Radiation Oncology, Gunma University School of Medicine,
Japan. takimoto@sb.gunma-u.ac.jp
To evaluate the treatment-related late sequelae including gonadal function and second
malignancy 94 patients with stage I and II testicular seminoma treated with
postorchiectomy radiation therapy were analyzed retrospectively. The 10-year cause
specific, disease free and actuarial survival rates were 100, 98.5 and 96.1% for stage II
and 91.7, 83.3 and 91.7% for stage II, respectively. The most common
late sequelae of gastrointestinal tract was peptic ulcer, developing in 16% of all
patients with a median interval of 12 months, but severity was mild except one who needed
subtotal gastrectomy. Second malignancies developed in 9 patients
(9.5%) with a median interval of 13 years, but calculated O/E ratio excluding 2
patients with secondary germ cell tumor of contralateral testis was 2.3 and did not reach
a significant level statistically. Concerning gonadal function assessed from the number of
the children, 79% of the patients who wanted to have children after the treatment were
successful in fathering children. No fatal complications were observed.
Radiotherapy for stages I and II
testicular seminoma: results and morbidity in 238 patients.
Vallis KA, Br J Radiol. 1995 Apr;68(808):400-5.
Department of Clinical Oncology, Western General Hospital, Edinburgh, UK.
We have undertaken a retrospective analysis of 238 patients with Stages I and II seminoma
of the testis treated with radiotherapy in Edinburgh between 1974 and 1989. There were
five deaths from seminoma. Cause-specific survival for the whole group at 2 and 5 years
was 99.2% and 98.1%, respectively. Cause-specific survival at 2 and 5 years by stage
(Royal Marsden staging classification) was: Stage I, 99.5% and 98.7% and Stage II, 98.1%
and 96.1%. Fourteen (5.9%) patients relapsed (one after treatment for his second
testicular seminoma). Eight were given successful salvage treatment, five died of seminoma
and one died of intercurrent disease. 13 (5.5%) patients developed
World Health Organisation (WHO) grade 3 gastrointestinal or haematological toxicity and
two developed grade 4 gastrointestinal toxicity as a result of abdominal radiotherapy. 22
patients (9.2%) developed problems ascribed to late morbidity of abdominal radiotherapy
including 18 with peptic ulcer disease. Contralateral testicular tumours occurred in seven
(2.9%) patients and five (2.1%) patients developed malignancies at other sites.
Long-term evaluation of postorchiectomy
radiotherapy for stage II seminoma.
Whipple GL, Am J Clin Oncol. 1997 Apr;20(2):196-201.
Radiation Oncology Department, SUNY Health Science Center, Syracuse, New York 13210,
U.S.A.
PURPOSE: To determine survival, long-term tumor control, and the effects of irradiation
for stage II seminoma. MATERIALS AND METHODS: Forty-five patients with stage II testicular
seminoma were treated between 1966 and 1989. There were 31 patients with stage IIA disease
and 14 with stage IIB disease. All patients underwent orchiectomy followed by iliac and
paraaortic irradiation (median dose: 30 Gy), with 37 patients receiving prophylactic
mediastinal and supraclavicular irradiation (median dose: 30 Gy). Follow-up ranged from 6
months to 20.6 years, with a median of 9.4 years. RESULTS: Uncorrected survival was 98% at
5 years, 84% at 10 years, and 79% at 15 years. Survival corrected for intercurrent disease
was 98% at 5, 10, and 15 years. Five patients developed recurrences with four successfully
salvaged by chemotherapy and/or irradiation. There were no serious
acute toxicities, and no late complications have developed from infradiaphragmatic
irradiation. Supradiaphragmatic irradiation was associated with an increased risk
of coronary artery disease compared to the age-matched general population. CONCLUSION:
Radiotherapy remains an effective treatment for stage II testicular seminoma, with a 98%
adjusted survival rate at 15 years, without serious acute toxicity. Supradiaphragmatic
irradiation should not be used in stage IIB patients for whom salvage chemotherapy is an
option. |