 |
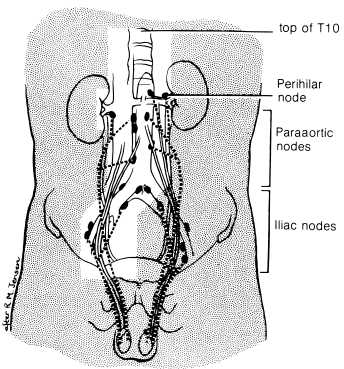
Radiation Therapy Techniques (from Perez) Patients with stage I seminoma should receive megavoltage irradiation to the paraaortic and ipsilateral pelvic nodes (Fig on left). The treatment volume should include the superior plate of the T10 vertebra and should extend inferiorly to the top of the obturator foramina. It is unnecessary to include the scar in the inguinal region. The lateral borders should include the paraaortic lymph nodes, as visualized by lymphogram, and the ipsilateral renal hilum. The field is usually 10 to 12 cm wide except at the hila, where it may be wider. The ipsilateral iliac and pelvic nodes should be encompassed by a shaped field with 2-cm margins on the visualized nodes. Testicular shielding should be used if the patient wishes to preserve fertility. The irradiation technique used is an anterior and posterior parallel opposed pair, using megavoltage equipment. Both fields should be treated daily, 5 days per week, Monday to Friday. It was agreed at the 1989 Consensus Conference that the recommended dose prescription should be 25 Gy given in 20 fractions. It is common practice in the United States to deliver about 25 Gy in 1.6- to 1.8-Gy fractions. Many centers commonly use higher doses, but all available data suggest that higher doses are unnecessary for sterilizing microscopic retroperitoneal disease |