The problem in deciding between treatment options for prostate cancer is
the diversity of choices from doing nothing at all (called surveillance or watchful
waiting) to radical surgery to radiation (some one would consider this is an intermediate
choice.)
Surveillance is based on the fact that prostate cancer can be
found in the prostate of men who die of old age in 60-80% of the men, and yet only 15-18%
of men get prostate cancer as a disease. (There is an expression "more men die with
it than of it".) The controversy about screening is based on the fact that some of
the men who have a PSA test and are diagnosed and treated for prostate cancer, would have
done just as well (with less side effects) if they had never been treated. A study on
surveillance showed that for slow growing tumors (well differentiated or low Gleason
score) who were not treated, the percent of men who would die of the disease would be
small (9% by 10 years and 9% by 15 years.) More lives would be lost with faster growing
tumors, moderate grade (24% by 10 years and 28% by 15 years) and poorly differentiated
(46% by 10 years and 51% by 15 years, from Albertsen JAMA 1995;274:626.)
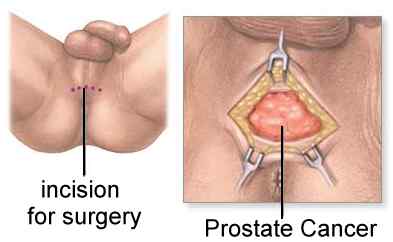
For patients with a long life expectancy and a more rapid growing cancer, treatment
(either surgery or radiation) is generally recommended. Traditionally for men 69 or
younger surgery was chosen (based on the belief that the long
term cure rate was higher) and for age 70 or older radiation
(based on the assumption that radiation was as good as surgery for at least 10 year
survival and less risky than surgery in older patients.) In the past it was argued that
the cure rates with surgery were better than with radiation. But if comparisons are mades
based on similar lveleles of PSA or grade (Gleason score) of the cancer, the results are
the same. A recnet study from MD Anderson (Cancer 2001;91:1414) showed that the results
after radical prostatectomy were quite poor if the PSA
level was high (prior to the operation) or the grade
(Gleason score) was high.Recently surgery has been used for older patients (based
on improvements in surgical technique making it safer and with lower side effects) but
radiation is also being used in younger patients (based on the belief that with more
modern techniques, e.g. 3-D or conformal external beam irradiation and the use of seed
implants, that the long term results are as good as surgery.)
The best proof of cure is for the man's PSA level to fall to a very low level (usually
0 after surgery and < 1 after radiation) and to remain at this low level for 10 years
or more. So far there is only a limited amount of data that compare similar stages of
prostate cancer, treated with the different forms of treatment, and that have measured the
PSA levels for 10 years or more. Some data is noted below. Some men assume that the cure
rates are the same and choose therapy based on the risks of different side effects. (In
general terms, surgery patients may have a higher risk of bladder problems or impotence,
and radiation patients more problems with their bowels.) Some complication comparisons are
noted below (additional information and comparisions of side effects can be found in the external beam section and seed section.) |