Gamma knife radiosurgery for hemangioblastomas:
clinical results and pathological findings
Wang EM, .Zhonghua Wai Ke Za Zhi. 2003 Jul;41(7):516-9.
Department of Neurosurgery, Huashan Hospital, Fudan University, Shanghai 200233, China.
OBJECTIVE: To retrospectively evaluate the effects of Gamma knife in the treatment of
cerebral hemangioblastomas. METHODS: From 1993 to 1996, seventeen patients with 29
hemangioblastomas were treated with Gamma knife. The patients mean age was 35 years
(range: 16 - 61 years). The mean tumor diameter was 16 mm (range: 6 - 55 mm).
Thirteen patients had recurrent or residual hemangioblastomas. Four with primary
hemangioblastomas were diagnosed using CT, MRI and DSA. The maximum dose to the tumors was
21.0 - 50.0 Gy, with mean dose of 33.7 Gy. The radiation dose to the periphery of tumors
was 12.0 - 24.0 Gy, with mean dose of 17.6 Gy. RESULTS: All the patients had been
followed up for 18 to 62 months, with mean 46 months. Five patients experienced clinical
improvement and reduction in tumor volume, and 5 remained stable and tumor unchanged in
volume during the follow-up period. Three patients died of tumor progression, surgery and
cancer after treatment 18, 22, 25 months respectively. Four patients underwent surgery
respectively at 3, 4, 29 and 48 months after gamma knife operation. The local control
rate of the tumors at 1 year was 92%, 2 years 88%, 3 years 80% and 4 years 75%.
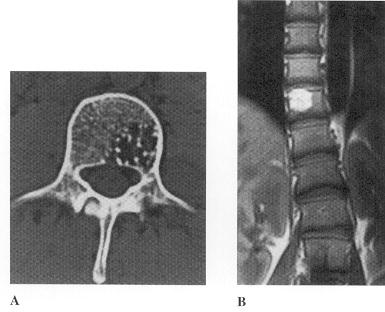
Pathological findings in these patients showed varying degrees of small vessel thickening
and occlusion together with degeneration, necrosis in the center of tumor and loss of
tumor cells at periphery. CONCLUSIONS: Gamma knife is not adequately reliable for the
control of hemangioblastoma cysts, it is an effective treatment of small or medium-size
solid tumors, but long-term follow-up is needed. The recommended dose is 16 to 20 Gy.
Gamma knife radiosurgery in 11 hemangioblastomas.
Niemela M, .J Neurosurg. 1996 Oct;85(4):591-6.
Department of Neurosurgery, Helsinki University Hospital, Finland.
One suprasellar, one mesencephalic, and nine cerebellar hemangioblastomas were treated
with the gamma knife in 10 patients (median age 48 years) in Stockholm between 1978 and
1993. Four patients had von Hippel-Lindau disease, a dominant inherited trait predisposing
to multiple hemangioblastomas. Six hemangioblastomas were treated with radiotherapy at a
median margin dose of 25 Gy (20-35 Gy) before 1990 and the next five with a median of 10
Gy (5-19 Gy). Computerized tomography or magnetic resonance images were available for 10
of the 11 hemangioblastomas at a median follow-up time of 26 months (4-68 months) after
radiosurgery. The solid part of six hemangioblastomas shrank in a median of 30 months,
whereas four hemangioblastomas were unchanged at a median of 14 months. Five
hemangioblastomas had an adjoining cyst and three of these cysts had to be evacuated after
radiosurgery. One solitary hemangioblastoma later developed a de novo cyst that also
needed evacuation. One patient with two cerebellar hemangioblastomas (margin dose 25 Gy
each) developed edema at 6 months and required a shunt and prolonged corticosteroid
treatment. The combined follow-up data of the 23 hemangioblastomas in 15 patients from
previous literature and the present series indicate that, first, a solitary
small- or medium-sized hemangioblastoma usually shrinks or stops growing after
radiosurgery. The recommended margin dose is 10 to 15 Gy. Second, the adjoining cyst often
does not respond to radiosurgery but requires later, sometimes repeated evacuation.
Treatment of hemangioblastomas in von Hippel-Lindau disease with linear
accelerator-based radiosurgery.
Chang SD, Neurosurgery. 1998 Jul;43(1):28-34
Department of Neurosurgery, Stanford University Medical Center, California 94305, USA.
OBJECTIVE: Stereotactic radiosurgery is increasingly being used to treat
hemangioblastomas, particularly those that are in surgically inaccessible locations or
that are multiple, as is common in von Hippel-Lindau disease. The purpose of this study
was to retrospectively evaluate the effectiveness of radiosurgery in the treatment of
hemangioblastomas. METHODS: From 1989 to 1996, 29 hemangioblastomas in 13 patients
with von Hippel-Lindau disease were treated with linear accelerator-based radiosurgery.
The mean patient age was 40 years (range, 31-57 yr). The radiation dose to the tumor
periphery averaged 23.2 Gy (range, 18-40 Gy). The mean tumor volume was 1.6 cm3
(range, 0.07-65.4 cm3). Tumor response was evaluated in serial, contrast-enhanced,
computed tomographic and magnetic resonance imaging scans. The mean follow-up period was
43 months (range, 11-84 mo). RESULTS: Only one (3%) of the treated hemangioblastomas
progressed. Five tumors (17%) disappeared, 16 (55%) regressed, and 7 (24%) remained
unchanged in size. Five of nine patients with symptoms referable to treated
hemangioblastomas experienced symptomatic improvement. During the follow-up period, one
patient died as a result of progression of untreated hemangioblastomas in the cervical
spine. Three patients developed radiation necrosis, two of whom were symptomatic.
CONCLUSION: Although follow-up monitoring is limited, stereotactic radiosurgery
provides a high likelihood of local control of hemangioblastomas and is an attractive
alternative to multiple surgical procedures for patients with von Hippel-Lindau
disease. |