| Medical literature
databases were searched for articles pertaining to pituitary adenomas and stereotactic
radiosurgery. A total of 35 peer-reviewed studies involving 1621 patients were
examined. Radiosurgery resulted in the control of tumor size in approximately 90% of
treated patients. The reported rates of hormone normalization for functioning adenomas
varied substantially. This was due in part to widespread differences in endocrinological
criteria used for the postradiosurgical assessment.
The risks of hypopituitarism,
radiation-induced neoplasia, and cerebral vasculopathy associated with radiosurgery
appeared lower than those for fractionated radiation therapy. The incidence of other
serious complications following radiosurgery was quite low. CONCLUSIONS: Although
microsurgery remains the primary treatment modality in most cases,
stereotactic
radiosurgery offers both safe and effective treatment for recurrent or residual pituitary
adenomas. In rare instances, radiosurgery may be the best initial treatment for patients
with pituitary adenomas. Further refinements in the radiosurgical technique
will likely lead to improved outcomes.
Gamma knife
radiosurgery for pituitary adenomas.
Izawa M, Hayashi M, Nakaya K, Satoh H, Ochiai T, Hori T, Takakura K. J Neurosurg
2000 Dec;93 Suppl 3:19-22
Department of Neurosurgery, Neurological Institute, Tokyo Women's Medical University,
Japan. mizawa@nij.twmu.ac.jp
One hundred eight patients with pituitary adenomas were treated over the last 7 years.
Seventy-four patients have been followed for more than 6 months and form the basis of this
report. CONCLUSIONS: Twenty-three patients harbored nonfunctioning adenomas, and 56
harbored functioning adenomas. The mean margin dose was 22.5 Gy (nonfunctioning adenomas,
19.5 Gy; functioning adenomas, 23.8 Gy).
Control of tumor growth was
achieved in 91%. A significant decrease of excessive hormone production was seen in 80% of
patients, and the endocrinological normalization rate was 30.3%. Postradiosurgical
complications were seen in 2.5%.
Gamma knife radiosurgery for pituitary tumors.
Jackson IM, Noren G. Baillieres Best Pract Res Clin Endocrinol Metab 1999
Oct;13(3):461-9
Department of Medicine, Rhode Island Hospital, Brown University School of Medicine,
Providence, USA.
Stereotactic radiosurgery with the gamma knife delivers focused radiation from a cobalt-60
source in a single session to a pituitary tumour with minimal radiation to the adjacent
normal brain tissue. Currently, gamma knife radiosurgery is predominantly used to treat
failed pituitary surgery, although it has a role as a primary treatment for patients
unwilling or unsuitable, for medical reasons, to undergo trans-sphenoidal surgery.
The major risk from gamma knife radiosurgery is radiation damage to the
visual pathways, but this can be avoided by limiting the radiation dose to the optic
chiasm to under 10 Gy. In contrast, the neuronal and vascular structures running in
the cavernous sinus are much less radiosensitive, allowing an ablative dose to be
administered to tumors showing lateral invasion and impinging on cranial nerves III, IV,
V and VI. Gamma knife radiosurgery appears to produce remission in secretory
tumors
faster than fractionated radiotherapy. Furthermore, the potential long-term risk of
developing a second extra-pituitary brain tumour, as well as the neuropsychiatric effects
associated with conventional radiation administration, seems less likely to occur with
this form of treatment.
Gamma knife radiosurgery for
prolactinomas.
Landolt AM, Lomax N. J Neurosurg 2000 Dec;93 Suppl 3:14-8
Gamma Knife Center, Klinik im Park, Zurich, Switzerland. 100023.1666@compuserve.com
OBJECT: In this retrospective investigation the authors examined the results of gamma
knife radiosurgery (GKS) for tumor remnants after unsuccessful open surgery and medical
treatment in 20 patients with prolactinomas. Particular attention is paid to a possible
radioprotective action of dopamine agonists similar to the action of octreotide in
acromegaly. METHODS: Twenty patients with prolactinomas were followed after GKS. Five
patients were treated successfully; their prolactin (PRL) levels dropped into the normal
range and dopaminergic drugs could be discontinued. Two spontaneous pregnancies were
observed and 11 patients experienced improvement. Improvement was defined as normal PRL
levels with the continued possibility of reduced medical treatment or a substantially
reduced medical treatment dose with some degree of hyperprolactinemia maintained. The
treatment failed in three patients who experienced no improvement. Patients treated with
dopaminergic drugs during GKS did significantly less well in comparison with the untreated
group when a cumulative distribution function (Kaplan-Meier estimate) was used.
CONCLUSIONS: The results of GKS for prolactinomas in this investigation are better than
the results published by others. This may be an effect of case selection because there
were no "salvage cases" in our group of patients. Because a dopamine agonist
seemed to induce radioprotection in this series, it is suggested that GKS be performed
during an intermission in drug therapy when the dopamine agonist is discontinued.
Gamma knife radiosurgery as a primary treatment for
prolactinomas.
Pan L, Zhang N, Wang EM, Wang BJ, Dai JZ, Cai PW. J Neurosurg 2000
Dec;93 Suppl 3:10-3
Department of Neurosurgery, Shanghai Gamma Knife Hospital, People's Republic of China.
nanzhang@sina.com
OBJECT: The purpose of this study was to estimate the efficacy of gamma knife radiosurgery
(GKS) in controlling tumor growth and endocrinopathy associated with prolactinomas.
METHODS: Between 1993 and 1997, 164 of 469 patients with pituitary adenomas treated by GKS
harbored prolactinomas. The dose to the tumor margin ranged from 9 to 35
Gy (mean 31.2
Gy), and the visual pathways were exposed to a dose of less than 10 Gy. The mean tumor
diameter was 13.4 mm. The mean follow-up time for 128 cases was 33.2 months (range 6-72
months). Tumor control was observed in all but two patients who underwent surgery 18 and
36 months, respectively, after GKS. Clinical cure was achieved in 67 cases. Clinical
improvement was noted with a decrease in the hyperprolactinemia after GKS. Nonetheless, in
31 (29%) of 108 patients who were followed for more than 2 years no improvement in serum
prolactin levels was demonstrated, although this could be normalized by bromocriptine
administration after treatment. Nine infertile women became pregnant 2 to 13 months after
GKS and all gave birth to normal children. There was no visual deterioration related to
GKS. Five women experienced premature menopause. In these patients there was subtotal
disappearance of the tumor and an empty sella developed. CONCLUSIONS:
Gamma knife
radiosurgery as a primary treatment for prolactinomas can be safe and effective both for
controlling tumor growth and for normalization of prolactin hypersecretion. A higher
margin dose (> or = 30 Gy) seemed to be associated with a better clinical outcome.
Gamma knife radiosurgery may make prolactinomas more sensitive to the bromocriptine.
Gamma knife surgery in pituitary microadenomas.
Park YG, Chang JW, Kim EY, Chung SS. Yonsei Med J 1996 Jun;37(3):165-73
Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Republic of
Korea.
The authors performed Gamma Knife radiosurgery in 27 patients with pituitary adenomas and
observed the hormonal changes after radiosurgery in 19 patients with functioning
microadenomas (5 with Cushing's disease, 7 with acromegaly, and 7 with prolactinoma). The
maximum dose administered ranged from 25 to 75 Gy. The margin of the tumor was encompassed
within the 50 to 90% isodose volume. The endocrinological status was assessed pre- and
post-operatively. We measured the serum growth hormone and prolactin level, as well as the
24-hour urinary free-cortisol level. Normalization of the hormonal level was achieved in 6
cases, the majority of them within 10 months. The other 6 cases showed marked reduction of
hormonal levels (less than 50% of preoperative levels) with a strong possibility of
hormonal remission at further follow-up. The remaining 6 were failures. The cure for one
case is still pending. It took approximately 1 approximately 3 months after the
radiosurgery before the reduction of hormonal secretion began to show up with some
improvement of symptoms. When the GKS was successful, hormonal secretion seemed to return
to normal within 10 months. Although further follow-up is necessary to evaluate the
long-term tumor control rate and hormonal effect, these initial results indicate a
potential therapeutic role of radiosurgery in controlling hormone hypersecretion in
pituitary microadenomas. Gamma knife radiosurgery is very promising in managing pituitary
microadenoma with complementary of the transsphenoidal surgery.
Stereotactic radiosurgery for pituitary adenoma invading
the cavernous sinus.
Shin M, Kurita H, Sasaki T, Tago M, Morita A, Ueki K, Kirino T. J Neurosurg
2000 Dec;93 Suppl 3:2-5
Department of Neurosurgery, The University of Tokyo Hospital, Japan.
shinmasa@ka2.so-net.ne.jp
OBJECT: The purpose of this study is to determine the efficacy of gamma knife radiosurgery
(GKS) treatment of pituitary adenomas that have invaded the cavernous sinus. METHODS:
Sixteen patients were treated with GKS: three with nonfunctional adenomas and 13 with
hormone-secreting (seven growth hormone [GH] and six adrenocorticotropic hormone [ACTH])
adenomas. More than 16 Gy and 30 Gy were delivered to the tumor margin for nonfunctioning
tumors and functioning tumors, respectively, keeping the dose to the optic pathways below
10 Gy. The median follow up was 3 years. Tumor growth control was achieved in all cases.
In GH-producing tumors, four of six cases evaluated were endocrinologically normalized
(serum GH < 10 mIU/L, somatomedin C < 450 ng/ml), and the remaining two cases also
showed a steady decrease in the GH and somatomedin level. In ACTH-producing tumors, three
of six cases were endocrinologically normalized (24-hour urinary-free cortisol < 90
mg/day), two were unchanged, and one showed hormonal recurrence 3 years after
radiosurgery. Notably, there were no cases of permanent hypopituitarism or visual symptoms
caused by radiosurgery. CONCLUSIONS: The authors data indicate that GKS can be a safe
salvage therapy for invading pituitary adenomas, with effectiveness equivalent to
conventional radiation therapy but with less risk of causing radiation-induced injury to
the surrounding structures.
The role of gamma knife radiosurgery in the management of
pituitary adenomas.
Thoren M, Hoybye C, Grenback E, Degerblad M, Rahn T, Hulting A L. J Neurooncol
2001 Sep;54(2):197-203
Department of Endocrinology and Diabetology, Karolinska Hospital and Institute, Stockholm,
Sweden.
No treatment modality has been entirely successful in the management of pituitary
adenomas. Although most patients with pituitary microadenomas can be cured by
transsphenoidal surgery, the results are less satisfactory in macroadenomas in particular
with suprasellar and/or parasellar extension. Additional treatment is then called for.
Conventional fractional radiotherapy can often control tumour growth but is limited to
45-50 Gy with a very slow reduction in elevated pituitary hormones and a high incidence of
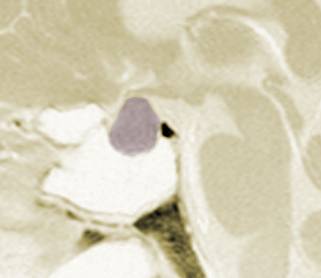
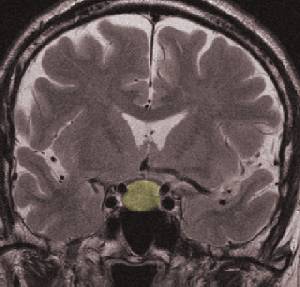
pituitary insufficiency. Stereotactic radiosurgery allows the delivery of radiation with
high precision to the target with low doses to the surrounding tissues permitting higher
radiation doses. Gamma knife radiosurgery using photon energy with gamma beams from
multiple cobalt 60 radiation sources is now used in many centers. It can be carried out in
an outpatient setting with one single treatment.
A more rapid normalization of pituitary
hormone hypersecretion than with conventional radiation can be achieved as well as arrest
of tumour growth and reduction of tumour mass. We therefore consider
gamma knife radiosurgery as a valuable compliment to pituitary surgery.
Long-term
prospective studies are needed to evaluate the frequency of pituitary insufficiency in
patients where the target area is determined with stereotactic magnetic resonance imaging
(MRI).
Gamma Knife radiosurgery as a primary surgical treatment
for hypersecreting pituitary adenomas.
Zhang N, Pan L, Dai J, Wang B, Wang E, Zhang W, Cai P. Stereotact Funct
Neurosurg 2000;75(2-3):123-8
Department of Neurosurgery, Hua Shan Hospital & Shanghai Gamma Knife Hospital,
Shanghai, China. nanzhang@sina.com
OBJECT: To estimate the efficacy of Gamma Knife radiosurgery (GKR) especially as a primary
surgical treatment for hypersecreting pituitary adenomas. METHODS: 274 patients were
treated with GKR. The mean tumor volume was 1.86 cm(3). The
mean peripheral dose was 28.7
Gy. RESULTS: 223 patients were followed up for an average of 31.6 months. The dose related
to the tumor growth control and endocrinological normalization was detailed and
statistical analysis of the data was performed. CONCLUSION:
GKR as a primary surgical
treatment for hypersecreting pituitary adenomas may be safe and effective |