Skin Cancer of the Eyelid (see review here)


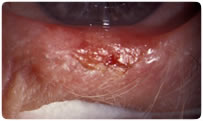
basal cell
basal cell
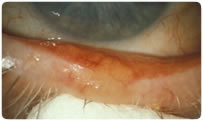
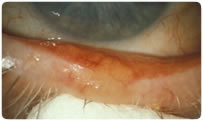
squamous
sebaceous
Skin Cancer of the Eyelid (see review here)


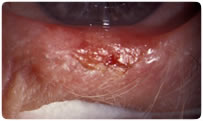
basal cell
basal cell
squamous
sebaceous
|
Eyelid Basal and Squamous Cell Carcinomas
In the treatment of basal cell and squamous cell
carcinomas of the eyelids,
radiation therapy can achieve an overall 90% to 95% cure rate.
After the diagnosis is confirmed by biopsy, 50 to 60 Gy (depending
on histology and size of the tumor) can be delivered by photon or
electron-beam techniques. An internal eye shield may be used to
protect the globe. Although surgery is the treatment of choice,
radiation therapy may be able to provide more acceptable cosmetic
outcome in selected cases while providing similar cure rates.
Radiation Therapy for Squamous Cell Carcinoma of the Eyelid IJROBP Volume 66, Issue 3, Supplement, Page S441 (1 November 2006) To evaluate the natural history and outcomes following radiation therapy for patients presenting with squamous cell carcinoma of the eyelid. Between 1950–2005, 39 patients with 42 tumors were treated with radiation therapy for squamous cell carcinoma of the eyelid at MDACC. Thirty-two eyelid tumors were treated with definitive radiation therapy and 10 tumors were treated with postoperative radiation therapy after wide local excision. The 5-year DSS and OS for all patients was 86% and 71%, respectively. Five-year DSS for patients treated with definitive radiation therapy and post-operative radiation therapy were 90% and 68%, respectively (p=0.36). In the post-operative group, one patient with a positive margin recurred locally at 16 months, and one patient developed distant metastases at 31 months. At 5 years, local control (LC), regional control (RC) and distant control (DC) were 88%, 94% and 97%, respectively, for all tumors. There was no difference in LC, RC and DC between definitive radiation therapy and postoperative radiation therapy group (88%, 93%, 97% and 85%, 100%, 97%, p =0.91). Five tumors (11.9%) failed locally at the eyelids. Of these 5 tumors, 2 tumors failed in both eyelids and ipsilateral regional nodal areas (1 parotid node and 1 mid jugular node). Five percent of the tumors from the eyelid had ipsilateral parotid metastases at presentation, and these patients were treated with surgery followed by radiation therapy to the primary site and ipsilateral neck. There were no regional failures in the four patients who received post-operative ipsilateral neck radiation. Five percent of patients who did not receive ipsilateral neck radiation failed regionally (1 ipsilateral parotid node, 1 ipsilateral mid jugular node). Distant metastasis occurred in 2% of all patients. No high risk factors, including positive margins, perineural invasion, lymphovascular invasion, or number of positive lymph nodes predicted for a decrease in locoregional control or distant metastasis following radiation therapy. Five percent of patients developed major complications including retinopathy, glaucoma, and nasolacrimal duct obstruction. Conclusions Radiation therapy has a high likelihood to control primary squamous cell carcinoma of the eyelid in both the definitive and postoperative setting. Ipsilateral neck irradiation following surgery achieves a high rate of regional control in patients presenting with nodal metastases. |