| Polyps occur universally in those with familial adenomatous polyposis, an
autosomal dominant hereditary condition, but this disorder accounts for only 1 percent of
cases of colorectal cancer. Adenomatous polyps are found in approximately 33 percent of
the general population by the age of 50 years and in approximately 50 percent by the age
of 70 years. There is more interest in COX-2 inhibitors like Celebrex
(go here). There are two COX genes in humans and COX-2 is not detected in healthy
epithelial cells but is expressed after induction by cytokines and is overly expressed in
many cancer cells.) There is also evidence that statins may prevent colon cancer.
(In a large study people taking statins for 5 years had a 51% reduction in colorectal
cancer , both drugs simvastin (Zocor) or pravastatin (Pravachol) were equally effective.)
Summary of Prevention from the NCI (go
here.)
High Fat Diet. Epidemiologic, experimental (animal),
and clinical investigations suggest that diets high in total fat, protein, calories,
alcohol, and meat (both red and white) and low in calcium and folate, are associated with
an increased incidence of colorectal cancer.
Fiber, Fruits, and Vegetables. Cereal fiber supplementation
and diets low in fat and high in fiber, fruits, and vegetables, however, do not reduce the
rate of adenoma recurrence over a 3-year to 4-year period.
Nonsteroidal Anti-Inflammatory Drugs. Nonsteroidal
anti-inflammatory drugs including piroxicam, sulindac and aspirin may prevent adenoma
formation or cause adenomatous polyps to regress in individuals with prior colorectal
cancer or adenomatous polyps and in the setting of familial adenomatous polyposis.
Cigarette Smoking. Cigarette smoking is associated with an
increased tendency to form adenomas and develop colorectal cancer.
Postmenopausal Hormone Use. Postmenopausal female hormone use
is associated with a decreased risk of colon cancer but not rectal cancer.
Colonoscopy. Colonoscopy with removal of adenomatous polyps
may reduce the risk of colorectal cancer.
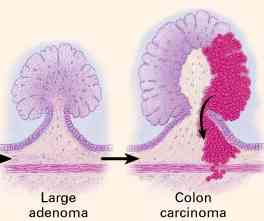
Molecular analyses of colorectal adenomas and carcinomas have led to a genetic model of
colon carcinogenesis, in which the development of cancer results not from any single
genetic event but from the accumulation of a number of genetic alterations By interfering
with these molecular events, chemoprevention could inhibit or reverse the development of
adenomas or the progression from adenoma to cancer. Recent studies have suggested the
potential of this approach in patients with familial adenomatous polyposis as well as in
persons with no known genetic syndrome but with a history of sporadic polyps. As evidence
emerges of the efficacy of chemoprevention in persons at high risk for colorectal cancer,
it seems appropriate to consider a similar strategy for the general population.
Although the treatment of advanced colorectal cancer continues to improve, large-bowel
cancer remains a major cause of illness and death. Recent observations suggest that
aspirin and other NSAIDs, supplemental folate and calcium, and postmenopausal
hormone-replacement therapy (estrogen) have a che mopreventive benefit. Since the value of
such prophylactic strategies has not yet been confirmed in double-blind,
placebo-controlled, randomized studies, chemoprevention cannot yet be accepted as standard
medical practice. Chemoprevention should not replace periodic fecal occult-blood tests and
endoscopic screening, as well as modification in known risk factors for colorectal cancer,
such as reduction in the intake of red meat, appropriate exercise, smoking cessation, and
weight control.
Any protective benefit must also be balanced against the potential side effects of the
long-term ingestion of any putative chemopreventive agent, including the gastric
irritation and platelet dysfunction associated with aspirin and other NSAIDs, which are
thought to be due to the inhibition of COX-1. More selective COX-2 inhibitors, such as
celecoxib and rofecoxib, have already been evaluated in patients with familial adenomatous
polyposis and are now being studied in patients with a history of sporadic polyps. In
addition, other potential chemopreventive agents, such as ursodiol (a modulator of bile
acid composition), (eflornithine (which inhibits cellular proliferation by altering
polyamine metabolism), and oltipraz (an inducer of the mutagen-detoxification enzyme
glutathione S-transferase), are undergoing evaluation in studies in animals and clinical
studies.
from The New England Journal of Medicine -- June 29, 2000 -- Vol. 342,
No. 26 |