What Vitamins
Should I Be Taking, Doctor?
Walter C. Willett, M.D., Dr.P.H., and Meir J. Stampfer, M.D., Dr.P.H. NEJM 2001;345:1819
Medical teaching has been that, in generally healthy
persons, nutritional needs can be readily met by diet alone. Public
interest in vitamin supplements is enormous, with 30 percent of the population
of the United States currently using such supplements.Political pressures have
led to a highly unregulated industry with limited control by the Food and Drug
Administration over marketing and quality.
Because foods contain many nutrients, distinguishing among the effects of
various nutrients in the same foods can be difficult. For example, the
observation that high-dose beta carotene supplementation in smokers did not
reduce the risk of lung cancer and may even have increased risk highlights the
potential dangers of extrapolating from epidemiologic studies of food
consumption (the consumption of fruits and vegetables, in this case) to
concentrated forms of a single chemical. Epidemiologic studies of
vitamin-supplement use per se are more directly relevant, but careful
statistical adjustment for other lifestyle factors is essential because users
of supplements may have healthier behavior in general than nonusers. We briefly
review the potential effects of commonly used vitamins, recognizing that the
relevant literature is far greater than what can be cited here.
Folic Acid
Several epidemiologic studies have found that periconceptional folic acid
supplementation is associated with a substantially reduced risk of neural-tube
defects. In a randomized trial, a high-dose folic acid supplement reduced the
incidence of recurrent neural-tube defects by 70 percent. A randomized trial
of a multivitamin that included folic acid (800 µg daily) in pregnant women
without a history of an affected pregnancy was stopped early because of a clear
benefit. This is the only definitively proven benefit of a multivitamin.
Although this relation has not been tested in randomized trials, substantial
evidence suggests that low folic acid intake increases the
risk of cardiovascular disease and several types of cancer.
Higher intake of folic acid is associated with a lower risk of colon
cancerand breast cancer, particularly among persons who are at increased risk
because of daily alcohol consumption. Also, a polymorphism in the gene for
methylenetetrahydrofolate reductase (which is involved in folate metabolism)
has been associated with an increased risk of colon cancer in some studies,
providing additional evidence that the relation between low folic acid
intake and an increased risk of colon cancer is causal. Alcohol interferes with
folate absorption and metabolism, perhaps accounting for increased folate
requirements among drinkers.
The optimal folic acid intake remains uncertain. An intake of 400 µg per
day minimizes blood homocysteine levels in most people, but more may be needed
to reduce the risk of cancer. Although an intake of 400 µg of folate per day
may be achieved by eating natural foods, the average American intake from
these sources is about 200 µg per day. Since 1998, the food-fortification
program in the United States has been adding about 100 µg per day. Thus, most
people in this country still consume less than 400 µg per day, and users
of multivitamins still have lower homocysteine levels than nonusers.
Vitamin B6
Vitamin B6 intake below the U.S. recommended daily allowance (RDA)
of 2 mg is associated with an increased risk of coronary disease, but it is
unclear whether this association is independent of folic acid intake.
Vitamin B12
Low blood levels of vitamin B12 (serum cobalamin level, <258 pmol
per liter), caused primarily by reduced absorption in elderly persons with low
gastric acidity, are also associated with higher blood homocysteine
levels.Twelve percent of elderly persons may have inadequate vitamin B12
stores. The consequences of marginal vitamin B12
status remain unclear, but they may include increased risks of vascular disease and cancer.Crystalline vitamin
B12, the form that is used in supplements, does not require gastric
acid for absorption, so a multivitamin can ensure that intake is adequate for
most people.
Vitamin D
Sun exposure alone can provide adequate vitamin D, but in the northern
United States, ultraviolet radiation during the winter is insufficient to
minimize the risk of osteoporosis and fractures.Among patients admitted to a Boston
hospital, 57 percent were deficient in vitamin D. Reasonable evidence
suggests that many Americans would benefit from supplemental vitamin D to reach
the RDA of 400 IU, and double this amount may be desirable for some
persons. A vitamin D intake of up to 2000 IU per day is believed to be safe.
Vitamin A
Because vitamin A helps regulate cell differentiation,
higher intakes could potentially reduce the risk of
cancer. However, blood levels are tightly controlled, and greater intake
in well-nourished persons has only a minimal effect on these levels. Both
intake and blood levels of vitamin A have generally been shown to be unrelated
to the risk of cancer.Supplemental beta carotene, a vitamin A precursor, has
consistently failed to reduce the risk of cancer in randomized trials.
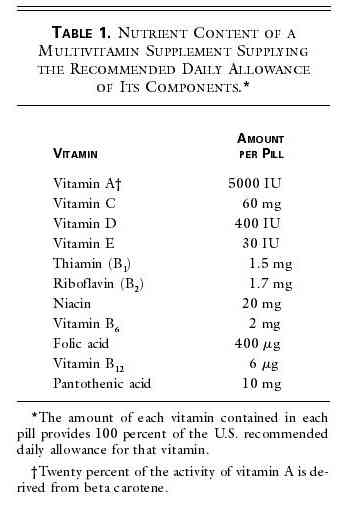
Multivitamin Preparations
The most common supplements are multivitamins that
typically include the RDA of thiamin, riboflavin, niacin, folic acid, and
vitamins A, C, B6, B12, D, K, and E. Few studies have
evaluated the effects of multivitamins per se rather than specific components
of them. In prospective studies, the daily use of a multivitamin has been
associated with a lower risk of coronary disease,colon
cancer,and breast cancer, particularly among regular consumers of
alcohol.In a randomized trial involving elderly persons, a
multivitamin–multimineral combination reduced the number of days of
illness due to infections by half.A similar supplement reduced the incidence of
stroke, primarily among men, in a nutritionally deficient population in
China.These results must be replicated in other settings.
Vitamin E Supplements
Vitamin E supplements, most of which contain 200 to 800 IU, lead to intakes
far greater than the RDA of 30 IU and well beyond those attainable by diet.
High doses of vitamin E block the oxidative modification of low-density
lipoprotein cholesterol and have additional effects that might reduce the risk
of coronary disease.However, the value of vitamin E for the prevention of
cardiovascular disease is controversial. In prospective, observational studies
involving persons without known cardiovascular disease, the use of vitamin E
supplements for two or more years — most commonly at a dose of 400 IU per
day — has been associated with a 20 to 40 percent reduction in the risk
of coronary disease.The long-term benefits of vitamin E supplementation for
primary prevention remain unclear.
It has also been hypothesized that vitamin E supplements reduce
the risk of cancer. No benefit has been found in terms of the risk
of breast cancer, and data on the risk of colon cancer are mixed.The randomized
Alpha-Tocopherol Beta Carotene Cancer Prevention Study found an unexpected,
significant reduction in the incidence of prostate cancer but not in the
incidence of other types of cancer. Because many cancer sites were examined,
this may represent a chance finding. Sparse evidence suggests that
vitamin E may slow the progression of Alzheimer's disease.
Vitamin C Supplements
Little evidence supports the existence of a benefit of vitamin C
supplementation beyond the range of the typical diet in the United States or
the current RDA of 90 mg for men and 75 mg for women (35 mg higher for
smokers), and minimal effects might be expected from supplementation because
tissues become saturated at about these levels of intake.Many studies have
found an association between a low dietary intake of vitamin
C and an increased risk of stomach cancer,but the
effects of vitamin C supplements have not been specifically evaluated. Even
long-term supplementation with vitamin C was not associated with a lower risk
of breast cancer. Fewer data are available on associations with other types of
cancer, but there is no compelling evidence of a benefit.
Few of the many possible associations between specific vitamins and specific
diseases have been examined in randomized clinical trials. The evidence that
folic acid reduces the risk of coronary disease and of colon cancer is strong,
although not definitive. The Food and Nutrition Board of the Institute of
Medicine notes that there has been no resolution of the question regarding the
effect of antioxidant vitamins on the risk of chronic disease.
Conclusions and Recommendations
Given the greater likelihood of benefit than harm, and considering the low
cost, we conclude that a daily multivitamin that does not
exceed the RDA of its component vitamins makes sense for most adults.
Substantial data suggest that higher intakes of folic acid, vitamin B6,
vitamin B12, and vitamin D will benefit many people, and a multivitamin
will ensure an adequate intake of other vitamins for which the evidence
of benefit is indirect.A multivitamin is especially important for women who
might become pregnant; for persons who regularly consume one or two alcoholic
drinks per day; for the elderly, who tend to absorb vitamin B12
poorly and are often deficient in vitamin D; for vegans, who require
supplemental vitamin B12; and for poor urban residents, who may be
unable to afford adequate intakes of fruit and vegetables.
Many multivitamins also include essential minerals, although the doses of
some of these minerals, such as calcium, are well below the RDA. Although we
have not discussed minerals here, there is less evidence supporting the
existence of a benefit for mineral supplements, with the exception of the
additional iron required by some premenopausal women. A vitamin pill
is no substitute for a healthful lifestyle or diet, because foods contain
additional important components, such as fiber and essential fatty acids. In
particular, a vitamin supplement cannot begin to compensate for the massive
risks associated with smoking, obesity, or inactivity. We also believe that
vitamin E supplements are reasonable for most middle-aged and older Americans
who are at increased risk for coronary disease. Evidence is still accruing, but
even assuming a low probability that vitamin E will eventually be proved
efficacious (and we view the probability as fairly high), the likelihood of
a benefit would still outweigh the very low probability of harm. We would offer a vitamin E supplement in a dose of 400 IU as an
option. Finally, although we do not recommend additional vitamin
supplements at present, the relevant evidence remains far from complete.
 |
![]()