from the NCI:
The term thymoma is customarily used to describe neoplasms that show no overt atypia of
the epithelial component. A thymic epithelial tumor that exhibits clear-cut cytologic
atypia and histologic features no longer specific to the thymus is known as a thymic
carcinoma (also known as type C thymoma).
Invasive thymomas and thymic carcinomas are relatively rare
tumors, together representing about 0.2% to 1.5% of all malignancies. Thymic
carcinomas are rare and have been reported to account for only 0.06% of all thymic
neoplasms. In general, thymomas are indolent tumors with a tendency toward local
recurrence rather than metastasis. Thymic carcinomas, however, are typically invasive,
with a high risk of relapse and death.
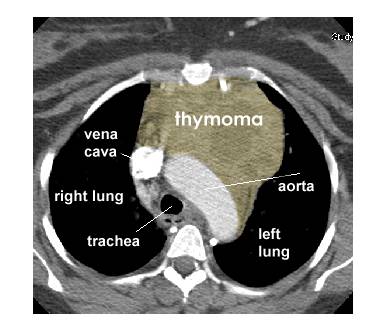
Most patients with thymoma or thymic carcinoma are aged 40 through 60 years.The etiology
of these tumors is not known. In about half of cases, thymomas/thymic carcinomas are
detected by chance with plain-film chest radiography.Ninety percent occur in the anterior
mediastinum.
Approximately 30% of patients with thymoma/thymic carcinoma are asymptomatic at the time
of diagnosis. In other cases, the presenting clinical signs of these tumors may include
coughing, chest pain, and signs of upper airway congestion. Paraneoplastic autoimmune
syndromes associated with thymoma include myasthenia gravis, polymyositis, lupus
erythematosus, rheumatoid arthritis, thyroiditis, and Sjögren’s syndrome, among
others. Autoimmune pure red cell aplasia and hypogammaglobulinemia each affect
approximately 5% of patients with thymoma. Thymoma-associated autoimmune disease involves
an alteration in circulating T-cell subsets. The primary T-cell abnormality appears to be
related to the acquisition of the CD45RA+ phenotype on naive CD4+ T cells during terminal
intratumorous thymopoiesis, followed by export of these activated CD4+ T cells into the
circulation.[12] In addition to T-cell defects, B-cell lymphopenia has been observed in
thymoma-related immunodeficiency, with hypogammaglobulinemia (Good syndrome) and
opportunistic infection.In contrast to thymoma, the association of thymic carcinoma and
autoimmune diseases is rare.
In a large retrospective study, approximately 47% of thymoma
cases (excluding thymic carcinoma) were found to be associated with myasthenia gravis.
Although the oncologic prognosis of thymoma is reported to be more favorable in patients
with myasthenia gravis than in patients without myasthenia gravis, treatment with
thymectomy may not significantly improve the course of thymoma-associated myasthenia
gravis.
Thymoma and thymic carcinoma should be differentiated from a number of nonepithelial
thymic neoplasms, including neuroendocrine tumors, germ cell tumors, lymphomas, stromal
tumors, tumor-like lesions (such as true thymic hyperplasia), thymic cysts, metastatic
tumors, and lung cancer.Standard primary treatment for these tumors is surgical, with en
bloc resection for invasive tumors if possible. Depending on tumor stage, multimodality
treatment includes the use of radiation therapy and chemotherapy, with or without surgery.
Thymoma has been associated with an increased risk for second malignancies, which appears
to be unrelated to thymectomy, radiation therapy, or a clinical history of myasthenia
gravis. Because of this increased risk for second malignancies and the fact that thymoma
can recur after a long interval, it has been recommended that surveillance should be
lifelong. The measurement of interferon-alpha and interleukin-2 antibodies has been
reported to be helpful in identifying patients with a thymoma recurrence.
Although the classification of thymomas remains a source of debate, some general
guidelines for a more coherent classification have emerged. The World Health Organization
pathologic classification of tumors of the thymus emphasizes the importance of independent
evaluations of the degree of tumor invasiveness and the tumor histology. Although some
thymoma histologic types are more likely to be invasive and clinically aggressive,
treatment outcome and the likelihood of recurrence appear to correlate more closely with
the invasive/metastasizing properties of the tumor cells. Therefore, some thymomas that
appear to be relatively benign by histologic criteria may behave very aggressively.
Independent evaluations of both the tumor invasiveness (using staging criteria) and tumor
histology should be combined to predict the clinical behavior of a thymoma.
Oncology (Huntingt) 1998 Jul;12(7):1001-5;
Natural history and treatment of malignant thymoma.
Cowen. Thymomas are rare, slow-growing neoplasms
that are considered to be malignant because of their potential invasiveness. Total resection followed by radiation therapy is the treatment of choice
for all thymomas, except stage IA tumors, which can be treated with surgery alone.
Chemotherapy can improve the outcome of invasive Masaoka stage III and IV thymomas or
recurrent thymomas. Only platinum-containing regimens show consistent efficacy.
Cancer 1998 Oct 15;83(8):1495-503
Thymoma: prognostic factors and
treatment outcomes.
Gripp. In Stages III and IV,
relapses were reduced by postoperative radiotherapy from 50% to 20%. The site of
relapse was outside the irradiated area in 80% of patients. Disease free survival and
median survival of patients with completely resected advanced thymomas did not differ from
that for patients with incompletely resected tumors who received radiotherapy.
CONCLUSIONS: Postoperative radiotherapy can improve local control in patients with
advanced thymoma. Survival after incomplete resection is not compromised when
postoperative radiotherapy is employed.
Cancer 1999 May 1;85(9):1871-84
Nonsurgical management of
malignant thymoma.
Hejna. Thymoma is a rare tumor entity. Surgery
remains the mainstay of treatment, but radiation and chemotherapy also have been applied
widely in both the adjuvant and the palliative setting. In the
adjuvant setting, radiation appeared to result in a higher survival rate compared with
historic controls as well as excellent local control in patients with advanced stage of
disease, whereas no apparent benefit was observed in patients with Masaoka et al.
classified Stage I disease. The large majority of chemotherapeutic studies were
case reports or Phase II trials of advanced disease, whereas no prospectively randomized
trials were performed. Response rates were relatively heterogeneous and ranged between 24%
and 100%, not including the results published in single case reports, and response rates
>50% have been found consistently with the application of polychemotherapy. In the
absence of randomized trials, multimodality approaches using induction chemotherapy
followed by resection and consecutive radiation have produced highly promising results in
terms of resectability and long term survival, even in patients with advanced disease.
Chest 1997 Oct;112(4 Suppl):296S-300S
Controversies in the management
of malignant thymoma.
Kohman. The management of most thymomas is
relatively straightforward: surgical resection remains the primary mode of therapy.
Conclusions include the following: invasiveness remains the single most consistent factor
in predicting outcome; surgery is the treatment of choice for thymoma whenever a complete
resection can be accomplished; and incomplete resection may have some advantage over
biopsy alone. The preponderance of evidence indicates that all
thymomas except completely encapsulated stage I tumors should be treated with
postoperative adjuvant radiation therapy in the hope of reducing the incidence of local
relapse. Myasthenia can no longer be considered an adverse prognostic factor in
thymoma; it may even confer a survival advantage, but this may be due to the preponderance
of early-stage tumors discovered incidentally in myasthenic patients. Other associated
autoimmune diseases confer a survival disadvantage. Demonstrating the equivalence of
minimally invasive thoracoscopic approaches to standard thymectomy will take many years of
investigation. Some promising reports on response to chemotherapy have led to the
development of a phase II intergroup study to assess the value of chemotherapy in advanced
thymoma.
J Clin Oncol 1997 Sep;15(9):3093-9
Cisplatin, doxorubicin, and
cyclophosphamide plus thoracic radiation therapy for limited-stage unresectable thymoma:
an intergroup trial.
Loehrer.Patients with a histologic diagnosis of
limited-stage unresectable thymoma or thymic carcinoma were eligible. Further requirements
included a Karnofsky Performance Score of > 60, no prior radiation to the chest, and
adequate bone marrow, hepatic, and renal function. No patient had undergone chemotherapy
previously. Patients received two to four cycles (repeated every 3 weeks) of cisplatin (50
mg/m2), doxorubicin (50 mg/m2), and cyclophosphamide (500 mg/m2) followed by a total
dosage of 54 Gy to the primary tumor and regional lymph nodes for patients with a stable,
partial, or complete response to chemotherapy. Among the 23 assessable patients, there
were five complete and 11 partial responses to chemotherapy (overall response rate,
69.6%). The median time to treatment failure was 93.2 months (range, 3 to 99.2+ months),
and the median survival time was 93 months (range, 1 to 110 months). The 5-year survival
rate is 52.5%. CONCLUSIONS: PAC combination chemotherapy produces response rates in the
management of patients with limited thymoma. Combined-modality therapy is feasible and
associated with prolonged progressive-free survival. The benefit of combined-modality
therapy over radiation therapy alone is suggested for patients with unresectable thymoma.
Int J Radiat Oncol Biol Phys 1995 Jun
15;32(3):651-9
Radiotherapy and chemotherapy for
invasive thymomas: a multicentric retrospective review of 90 cases. The FNCLCC trialists.
Federation Nationale des Centres de Lutte Contre le Cancer.
Mornex We retrospectively reviewed the outcome and
prognostic factors in a series of 90 patients presenting with an invasive thymoma treated
by partial resection or biopsy and radiation therapy. The median radiation dose to the
tumor was 50 Gy (30-70 Gy). Supraclavicular radiation was performed in 59 patients (median
dose 40 Gy). Chemotherapy, combined with radiation in 59 patients, consisted of multidrug
regimens, mainly platinum based. The 5- and 10-year overall survival rates are 51 and 39%,
respectively. There is a great impact of the extent of surgery on survival: the 5- and
10-year survival rates were 64% and 43%, respectively, after partial resection, compared
to 39% and 31% after biopsy. Local control at 8.5 years was obtained in 59 of 90 patients
(66%).There is a significant relationship between the extent of surgery and the local
control (16% of relapse after partial resection vs. 45% after biopsy). There is also a great impact of radiation on local control. However, the
rate of local recurrence (34%) justifies recommending a higher dose of radiation (> 50
Gy) than doses used in this study, for incompletely resected patients. The role of
chemotherapy needs to be further assessed.
Ann Intern Med 1998 Jul 15;129(2):100-4
A multidisciplinary approach to
therapy for unresectable malignant thymoma.
Shin.The treatment regimen consisted of induction chemotherapy (three courses of cyclophosphamide, doxorubicin, cisplatin,
and prednisone), surgical resection, postoperative radiation therapy, and consolidation
chemotherapy (three courses of cyclophosphamide, doxorubicin, cisplatin, and
prednisone). Disease responded to induction chemotherapy completely in 3 patients (25%)
and partially in 8 patients (67%); 1 patient had a minor response (8%). Eleven patients
had surgical resection; 1 refused surgery. Tumors were removed completely in 9 (82%) and
incompletely in 2 (18%) of 11 patients who had been receiving radiation therapy and
consolidation chemotherapy. All 12 patients are alive (100% at 7 years), with a median
follow-up of 43 months, and 10 patients are disease free (73% disease-free survival at 7
years).
S Afr J Surg 1997 Nov;35(4):206-9
Role of radiotherapy in stage III
invasive thymomas.
Sur.Twenty-five patients with malignant invasive
stage III thymomas who underwent biopsy for tissue diagnosis were treated with primary radiotherapy (mean dose 46.36 Gy, range 32.4-58 Gy). The 5-year disease-free survival was 81% overall survival 72% and
local failure rate 13%. Radical external beam radiotherapy alone can give good results in
malignant stage III invasive thymomas.
Int J Radiat Oncol Biol Phys 1996 May
1;35(2):357-60
Entire hemithorax irradiation
following complete resection in patients with stage II-III invasive thymoma.
Uematsu To evaluate the feasibility and efficacy
of prophylactic entire hemithorax irradiation (EH) in
addition to mediastinal irradiation (MRT) following a complete resection in Stage II-III
invasive thymoma. Forty-three patients with invasive thymoma treated with surgery and
radiation therapy between 1978 and 1993 were analyzed retrospectively. All 43 patients
underwent a complete surgical resection and were judged to have Masaoka's Stage II-III
invasive thymoma. Of these, 23 patients received EH and MRT (EH-MRT) and the remaining 20
received MRT. EH was 15 Gy per 15 fractions over 3 weeks (without lung compensation
calculation). In both the EH-MRT and MRT group, the total radiation doses to the
mediastinum were similar with a median of 40 Gy. Only one of the 23 patients with EH-MRT
relapsed. On the other hand, eight of the 20 with MRT relapsed, six of whom died of
disease. The pleura was the most common site of failure. At 5 years, the relapse-free rate
was 100% for those receiving EH-MRT and 66% for those with MRT (p = 0.03); the overall survival rate was 96% for those with EH-MRT, and 74% for those
with MRT. The only significant treatment-related complication was radiation
pneumonitis requiring treatment, in one patient who received MRT and three who received
EH-MRT, including one death of a 72-year-old man and one 68-year-old woman with severe
lung fibrosis. CONCLUSION: Except for elderly patients, EH-MRT following a
macroscopically complete resection appears to be safe and feasible, and can reduce
intrathoracic relapses.
Ann Thorac Surg 1997 Dec;64(6):1585-91; discussion
1591-2
Multimodality treatment of
thymoma: a prospective study.
Venuta We considered three groups. Group
I benign thymoma, included stage I and II medullary and stage I mixed thymomas;
radical resection with no adjuvant therapy was performed. Group II , invasive thymoma,
included stage I and II cortical and stage II mixed thymomas; postoperative chemotherapy
plus radiotherapy was always administered. Group III , malignant thymoma, comprised stage
III and IV cortical thymomas and stage III mixed thymomas; resectable stage III lesions
were removed, and highly invasive stage III and stage IV lesions underwent biopsy,
neoadjuvant chemotherapy, and surgical resection; postoperative chemotherapy and
radiotherapy was administered to all patients. The 8-year survival rate for patients in
stages I, II, III, and IV was 95%, 100%, 92%, and 68%, respectively. Group I had an 8-year
survival rate of 94%; group II, 100%; and group III, 76%. Survival
was compared with that of patients operated on before 1989: differences were not
significant for group I; survival improved in group II (100% versus 81%;); and group III
showed significant improvement (76% versus 43%). |