BACKGROUND: There still is debate as to whether breast carcinoma patients with isolated
supraclavicular recurrence should be considered to be patients with disseminated disease
or patients for whom aggressive treatment with curative intent is justified. METHODS: In
the period 1984-1994, 4669 patients with invasive breast carcinoma underwent axillary
dissection in 1 of 8 community hospitals in the southeastern part of the Netherlands.
During follow-up, 42 patients with isolated supraclavicular recurrence, without other
sites of distant disease, were identified. RESULTS: The median interval between
treatment of the primary tumor and diagnosis of the supraclavicular recurrence was 2.5
years (range, 0.2-11.5 years). Radiotherapy was administered to 25 patients (60%), 5
of whom also underwent surgery and 16 of whom also received chemotherapy or hormonal
therapy. Eleven patients received hormonal therapy only, and four received chemotherapy
only. One patient received surgical treatment only, and one patient remained untreated.
Complete remission was achieved in 35 patients (83%), but a second supraclavicular
recurrence occurred in 12 (34% of patients who achieved complete remission). Overall, 6
patients (14%) were alive without evidence of disease after a follow-up period of 4.4-8.3
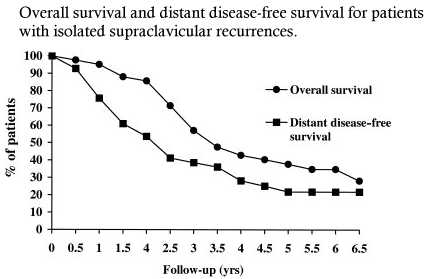
years. The 5-year actuarial overall survival and distant
disease-free survival rates, based on the date of diagnosis of supraclavicular recurrence,
were 38% and 22% respectively. The distant disease-free survival rate was
somewhat better for the 25 patients who underwent radiotherapy as part of the treatment
for supraclavicular recurrence than it was for the 17 patients who did not receive
radiotherapy (P = 0.06); the difference became more pronounced after the exclusion of 8
patients who had received axillary and supraclavicular radiotherapy as part of treatment
for the primary tumor (P = 0.002). CONCLUSIONS: Although complete remission can be
obtained in most patients with isolated supraclavicular recurrence, the prognosis for
these patients is poor. Involved field radiotherapy appears to play an important role
in the treatment of supraclavicular recurrence and may improve the distant recurrence-free
survival rate.
In the current study, the observed rate of isolated SR was 1.0% (42 of 4669 patients).
Taking into account these sources of incomplete follow-up, the actual rate of isolated SR
was estimated to be 1.5-2%. This rate is slightly higher than the 0.5% reported
by Halverson in a study of 511 patients with Stage I or II breast carcinoma.
Comparison with other published studies is hampered by differences among patient series
with respect to tumor stage and treatment. Many (older) studies reported much higher rates
of SR because they included relatively large proportions of patients with tumors larger
than 5 cm or locally advanced breast carcinoma, or patients without axillary dissection;
other studies were restricted to patients who underwent radical mastectomy or to patients
with node-positive breast carcinoma. In addition, unlike the current study, most other
studies were not restricted to isolated SR and instead included SR accompanying or
following other distant metastases. In the current study, the median interval between
first treatment for breast carcinoma and diagnosis of SR was 2.5 years, which is similar
to the mean interval of 26 months reported by Hirn-Stadler
The prognosis for patients with SR was poor. The published 5-year overall survival
rates for patients with isolated supraclavicular disease vary from 5% to 41%, with most
reported values between 20% and 30 %. The prognoses for patients with supraclavicular
metastases at first presentation and for patients with SR during the course of disease
seem comparable, although the two groups are not clearly separated in most studies. In a
previous analysis of 59 breast carcinoma patients with axillary recurrence after axillary
clearance, 5-year overall survival and distant recurrence-free survival rates were 39%
and 35% , respectively. These rates are only slightly better than the rates for
patients with SR in the current study. Fentiman compared the survival of 35 patients
with ipsilateral SR after radical mastectomy with the survival of patients with local skin
recurrences; the survival rate for the former group fell between the rate for patients
with 1 skin nodule and the rate for patients with multiple nodules. According to the
results of the current study and others, tumor control of supraclavicular disease is not
the main problem. Of the 42 patients in the current series, 35 (83%) achieved complete
remission, and 12 of these 35 (34%) experienced local progression during the follow-up
period; so in 23 of 42 patients (55%), a long-lasting, complete local remission was
achieved. The main problem for patients with SR is the development of metastases at more
distant sites. In the current study, the distant disease-free survival rate after 5 years
was only 22%. This finding indicates that in most cases, isolated SR is a precursor of
widespread disseminated disease. More than two-thirds of all patients developed bone
metastases, and it appears likely that these metastases already were present at the time
of diagnosis of SR. Routine evaluation of patients with SR using positron emission
tomography, a sensitive technique for detecting bone metastases, may be able to protract
the diagnosis of these metastases and therefore have a significant effect on treatment
planning.
There are no specific guidelines for the treatment of patients with SR. Treatment
is highly individualized and should be planned by a multidisciplinary team. In the current
study, more than half of all patients underwent multimodality treatment involving some
combination of surgery, radiotherapy, hormonal treatment, and/or chemotherapy. In the
univariate analysis, use of radiotherapy showed a borderline significant association with
development of metastases at more distant sites; i.e., patients with SR who received
radiotherapy were less likely than those who did not to develop metastases at distant
sites other than the supraclavicular region. One should note that this finding is based on
a nonrandomized study and may be explained in part by differences in prognostic factors
(e.g., prior irradiation) between those who received radiotherapy and those who did not.
We therefore performed a separate analysis that excluded all patients who had received
prior axillary and supraclavicular radiotherapy. Despite the limited number of patients in
this analysis, the patients who received radiotherapy exhibited a significantly better
distant recurrence-free survival rate than did patients who did not receive radiotherapy
to treat SR. A favorable effect due to radiotherapy also was reported by Abraham
in a series of 20 consecutive women with SR who received high-dose chemotherapy and
autologous blood stem cell support, significantly better progression-free survival was
observed among the 11 patients who received consolidative radiotherapy to the involved
supraclavicular region after transplantation. The median survival time for these patients
was 37 months, similar to the median of 41 months in the current study.
The optimal treatment strategy for SR is not yet known. Radiotherapy leads to reasonable
local control, but the value of systemic therapy is less clear. In the small randomized
trial of Pergolizzi which compared chemotherapy alone with induction
chemotherapy followed by radical radiotherapy the 5-year overall survival rates were
17% and 36%, respectively . Another small trial reported better disease-free survival
(but not better overall survival) after the addition of tamoxifen to radiotherapy in the
treatment of breast carcinoma patients who predominantly had chest wall recurrences or
skin metastases. Some authors recommend aggressive multimodality treatment because of the
relatively small tumor burden associated with supraclavicular disease.Brito from The
University of Texas M. D. Anderson Cancer Center, observed significantly better survival
after multimodality treatment among 70 patients with solitary ipsilateral supraclavicular
metastases at first presentation compared with patients with nonsupraclavicular metastatic
disease. Due to concerns regarding undertreatment, Brito et al. advocated the inclusion of
supraclavicular disease in the Stage III (rather than Stage IV) category. This
recommendation was followed by the International Union Against Cancer in the most recent
edition of the TNM Classification of Malignant Tumors; patients with metastases in
supraclavicular lymph nodes now are classified as N3c/pN3c, and a new stage (Stage IIIC)
that includes N3 (pN3a, pN3b, pN3c) M0 (any T-classification) has been introduced. In
previous editions, these malignancies had been classified as distant metastases (M1; Stage
IV disease).
Patients with SR have a poor prognosis, which probably is similar to the prognosis for
patients with supraclavicular disease at first presentation of breast carcinoma.
Nonetheless, the prognosis for patients with SR is slightly better than for patients with
metastatic disease at other sites. Involved field radiotherapy, in addition to systemic
treatment, appears to play an important role in achieving local control of disease and may
improve the distant recurrence-free survival rate.
Supraclavicular nodal relapse of breast cancer: prevalence, palliation,
and prognosis.
Ampil FL, Caldito G, Li BD, Burton GV.
Eur J Gynaecol Oncol. 2003;24(3-4):233-5. Department of Radiology, Louisiana State
University Health Sciences Center
PURPOSE: To determine the frequency, palliative effects of radiotherapy (RT) and survival
of patients developing supraclavicular nodal relapse (SNR) after definitive surgery for
non-disseminated breast cancer (BCa). METHODS: A retrospective study of individuals
treated by breast conserving surgery or modified radical mastectomy for Stage I to III BCa
at a single institution during a 17-year period (1980-96) was undertaken. RESULTS: Of the
536 patients studied, 22 (4%) developed SNR. Among the seven symptomatic women, the
complete subjective response rate after RT was 71%. Of the 18 evaluable patients with
manifest SNRs, tumor regression was complete in 12 (66.6%), partial in one (5.6%), and
absent in five (27.8%). The overall median survival was 11.5 months; five patients (23%)
survived for at least two years. CONCLUSION: Supraclavicular nodal relapse in breast
cancer patients occurs infrequently. The application of radiotherapy for palliation of SNR
was fully justified by the perceived results even though long-term survival was not often
observed.
The supraclavicular recurrence of breast carcinoma
Hirn-Stadler B. Strahlenther Onkol. 1990 Dec;166(12):774-7.
Universitatsklinik fur Strahlentherapie und Strahlenbiologie Wien.
Between January 1970 and December 1978 39 patients with isolated supraclavicular
recurrence of breast cancer were referred to the Department of Radiotherapy and
Radiobiology, University of Vienna. All patients have had mastectomy as primary treatment.
In 46% of the patients a surgical excision of involved lymph node has been performed
before irradiation. The median interval between mastectomy and supraclavicular
recurrence was 26 months. The cumulative incidence after three years was 75%. 15
patients have shown complete local response during the whole follow-up time. In 38
patients, osseous and/or visceral metastasis were observed after a median interval of
eight months. After two years, 87% of the patients presented distant disease. 15
patients suffered on local pain in the supraclavicular region or in the ipsilateral
shoulder with lymph oedema of the arm. The median survival after therapy was 18 months.
The death rate after three years was 77%. Patients with a recurrence-free interval after
mastectomy less than two years had a median survival time of eleven months whereas
patients with a recurrence-free interval had 26 months.
The role of radiotherapy in the treatment of supraclavicular lymph
node metastasis after radical mastectomy
Yamada T, Morita K. Nippon Igaku Hoshasen Gakkai Zasshi. 1991 Feb
25;51(2):155-61.
Department of Radiotherapy, Aichi Cancer Center.
To define the role of radiotherapy in the treatment of supraclavicular lymph node (SCN)
metastasis after initial surgery for breast cancer, a retrospective review of 55 patients
with ipsilateral SCN metastasis after (extended) radical mastectomy was undertaken. In
most cases, SCN metastasis is a manifestation of the systemic dissemination, because 87%
of the patients developed second recurrence in 2 years after radiotherapy to SCN. However,
the response to radiotherapy closely related to the survival after radiotherapy. 3
year-survival of the patients showing complete response was 42% while of the patients
showing partial response was 9%. Six out of 34 mastectomized patients with sole SCN
metastasis survived more than 3 years without evidence of recurrence following
radiotherapy to SCN. It can be suggested that radiotherapy to SCN metastasis is not always
palliative treatment, and has potency to improve the prognosis of the mastectomized
patients. The prognostic factor of the patients with SCN metastasis was also referred. The
time interval from initial surgery until SCN recurrence (disease free interval) has
prognostic significance, because it indicates the natural course of each tumor. Presence
of metastasis other than SCN at the time of first recurrence and poor response to
radiotherapy predict worse prognosis.
Ipsilateral supraclavicular lymph nodes metastases from breast cancer as only
site of disseminated disease. Chemotherapy alone vs. induction chemotherapy to radical
radiation therapy.
Pergolizzi S, Ann Oncol. 2001 Aug;12(8):1091-5.
Institute of Radiological Science, Department of Radiation Oncology University of Messina,
Italy. pergoste@solnet.it
BACKGROUND: To define the role of radiotherapy (RT) in the treatment of ipsilateral
supraclavicular lymph-nodes metastases (ISLM) from breast cancer as only site of
disseminated disease, we started a prospective non-randomized clinical trial in 1989. Here
we report the final results with a median follow-up of 8.75 years. PATIENTS AND METHODS:
Thirty-seven patients (pts), with ISLM from breast cancer, were consecutively enrolled
into two arms. Arm A (18 pts): chemotherapy (CT) for six courses. Arm B (19 pts): CT
for three courses followed by RT to the site of ISLM at 'radical' dose of 50-60 Gy.
RESULTS: In arm A, a median Time to Progression (TtP) of 7 months with a median Overall
Survival (OS) of 28 months was recorded. In comparison, patients in arm B had a longer
median TtP with 20 months as well as a better median OS with 41 months, respectively. An
actuarial five-year disease-free survival of 5.5% was obtained in arm A vs. 21% in arm B.
A statistically significant difference in TtP was demonstrated between the two groups (P =
0.01). CONCLUSIONS: These data demonstrate that a better event-free survival could be
achieved in patients with ISLM submitted to induction CT and radical irradiation. This
also translated into a longer survival although this did not achieve statistical
significance. We want to stress the importance of local control by RT since it does imply
that not all of these patients have micrometastases at the time of relapse in the
supraclavicular foss
High dose chemotherapy and autologous blood stem cell support in women with
breast carcinoma and isolated supraclavicular lymph node metastases
Rick Abraham, Cancer 2000;88:790-5.
The prognosis of patients with isolated supraclavicular lymph node (SCN) metastases is
similar to patients with metastatic breast carcinoma involving other sites. Because these
patients have a lower disease burden compared with women with distant metastases, their
outcome after high dose chemotherapy (HDCT) may be superior.
The authors evaluated event free survival (EFS) and overall survival in a series of 20
consecutive women with SCN metastases as the only site of metastatic disease who were
treated with HDCT and peripheral blood stem cell transplantation at The Toronto Hospital.
All patients had responded to 4-6 cycles of induction CT using either an
anthracycline-containing regimen or a single agent taxane, and received intensive therapy
comprised of mitoxantrone, 64 mg/m2; cyclophosphamide, 6000 mg/m2; and carboplatin,
800-2000 mg/m2, each divided over 4 days followed by the infusion of autologous peripheral
blood stem cells. Involved field radiation therapy (RT) was administered when possible
after transplantation to the supraclavicular fossa and tamoxifen was given to previously
untreated patients if they were hormone receptor positive or if their hormone receptor
status was unknown. At a median follow-up of 28 months, 13 of the 20 women were alive,
11 of whom (55%) remained in continuous complete remission. There were no
treatment-related deaths. The median overall survival was 37 months and the median
progression free survival was 32 months from the date of transplantation. Consolidative
RT was delivered to 11 women and on univariate analysis was found to be significantly
associated with better EFS The long term outcome of women with breast carcinoma and
isolated SCN metastases whose disease is sensitive to CT appears to be favorable; whether
this result is superior to that achieved with standard therapy alone remains to be
confirmed in prospective, randomized trials. |