|
Distal cT2N0 Rectal
Cancer: Is There an Alternative to Abdominoperineal Resection?
Ramesh Rengan, Bruce D. Minsky.
JCO Aug 1 2005: 4905–4912.
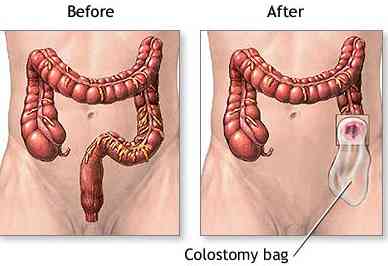
Patients with cT2N0 distal rectal cancer do
not require adjuvant therapy. However, when a patient refuses
an abdominoperineal resection (APR), is there an alternative?
The German CAO/ARO/AIO 94 preoperative versus postoperative
rectal trial reported that the incidence of sphincter
preservation in those patients who were judged clinically by
the operating surgeon to require an APR was significantly increased
in the preoperative (39%) versus postoperative arm (20%). Since
patients enrolled in that trial had either cT3, T4, and/or N+
disease, combined-modality therapy was necessary for adjuvant
therapy. In this report, we present the rates of sphincter
preservation and function, toxicity, local control, and
survival following preoperative pelvic radiation and selective
postoperative chemotherapy in patients with distal cT2N0 rectal
cancer who refused an APR.
The purpose of this trial is to
determine whether preoperative external-beam radiation therapy
can increase the rate of sphincter preservation for patients
with distal cT2N0 adenocarcinoma of the rectum. Between April
1988 and October 2003, 27 patients with distal rectal
adenocarcinoma staged T2 by clinical and/or endorectal
ultrasound who were judged by the operating surgeon to require
an APR were treated with
preoperative pelvic radiation alone
(50.4 Gy).
Surgery was performed 4 to 7 weeks later. If pathologic
positive pelvic nodes were identified, postoperative adjuvant
chemotherapy was recommended. The median follow-up was 55 months
(range, 9 to 140 months).
The pathologic complete response rate was 15% and
78% of patients
underwent a
sphincter-sparing procedure. The crude incidence of
local failure for patients undergoing a sphincter sparing
procedure was 10% and the 5-year actuarial incidence was 13%.
The actuarial 5-year survival for patients undergoing sphincter
preservation was as follows: disease-free, 77%; colostomy-free,
100%; and overall, 85%. Using the Memorial Sloan-Kettering Cancer
Center sphincter function score, 54% of those undergoing a
sphincter-sparing procedure had good/excellent bowel function
at 12 to 24 months after surgery, and 77% had good/excellent
function at 24 to 36 months after surgery. Our data
suggest that for patients with cT2N0 distal rectal cancer who
require an APR, preoperative pelvic radiation improves
sphincter preservation without an apparent compromise in local
control or survival.
Whole
pelvic field. The lateral borders were 2.0 cm lateral to the
widest bony margin of the true pelvic side walls. The distal
border was at the base of the obturator foramen or 1 cm below
the anus, whichever was lower. The superior border was at the
L5/S1 junction. The posterior field margin was a minimum of 1
cm behind the anterior bony sacral margin, and blocks were used
to spare the posterior muscle and soft tissues. The external
iliac nodes were not included in the lateral radiation fields.
The anterior margin was at the most posterior aspect of the
symphysis pubis. The anus was considered part of the target
volume; therefore, it was included in the whole pelvic field.
The whole pelvis plus the primary nodal groups at risk received
46.8 Gy. This was followed by a 3.6-Gy boost to the primary
tumor bed.
Boost
field. The intent of the boost was to treat the primary tumor
with a 3-cm margin and not to include the nodal groups.
Therefore, the exact size was determined by the size and
location of the primary tumor. In general, field sizes measured
10 x 10 or 12 x 12 cm, and corner blocks were used if possible.
Opposed lateral fields were used. The boost dose was 3.6 Gy;
therefore, the total dose (pelvis + boost) was 50.4 Gy. |