Polypectomy
Endoscopy and snare polypectomy provide a simple and cost-effective means of managing
colorectal polyps.In practice, all polyps should be considered for removal. Polyps that
are smaller than 5 mm, also referred to as diminutive polyps, usually are benign, rarely
produce bleeding, and may be left in place if they are multiple. But at least three to
five of the polyps should be removed for histologic examination they should all be removed
subsequently if found to be adenomas.
It often is not possible to determine the histologic type by gross visual appearance, but
polyps larger than 2 cm in size usually are adenomatous and should be removed in toto if
pedunculated. If sessile, they may need to be removed piecemeal, although the histologic
evaluation of the presence or degree of invasion of any carcinomatous foci would then be
difficult or impossible.If there is any concern that residual polyp tissue may be left,
the polypectomy site should be tattooed with sterilized India ink to facilitate follow-up
evaluation. This should also be done if there is a high index of suspicion that a polyp
may be malignant at the time of polypectomy, or as a secondary procedure after this has
been confirmed histologically, prior to definitive surgery if this is indicated. The
number of polyps that can be removed safely depends on their location and size. In the
patient with a diagnosis of FAP, colectomy, not polypectomy, is indicated. For multiple
adenomatous polyps, where there is the possibility of removing them endoscopically, the
colon should be cleared of polyps a section at a time to reduce the chance of
complications. The wall thickness of the cecal area and right colon is thinner than that
of the left, which also must be considered when removing polyps through cautery. If polyps
are inflammatory, hyperplastic, or otherwise nonadenomatous by histologic examination,
complete removal is unnecessary, but a sampling of several polyps from each cluster is
required, particularly if there is a suspicion of intercedent malignancy.
Polypectomy is safe in adults and children when performed by experienced physicians. The
major complication rate is less than 2%, the requirement for hospitalization or surgical
intervention less than 0.3%, and death is virtually nonexistent. Polypectomy should be
deferred in patients on aspirin or anticoagulation, or in those with severe bleeding
diatheses, unstable cardiac arrhythmias, recent myocardial infarction, acute colitis,
pregnancy (second or third trimester), recent colonic surgery, or abdominal abscess or
perforation.
When an adenoma is found, surveillance colonoscopy after 3 years suffices provided the
colonoscopist has reasonable confidence that polypectomy is complete, and adequate views
have been secured of the entire colon. If the repeat surveillance colonoscopy is clear at
a further 3 years, scheduling may be reduced to every 5 years. For patients at higher risk
for colorectal cancers, such as those at risk because of hereditary nonpolyposis
colorectal cancer, more frequent examinations may be in order. On the other hand, patients
with only small tubular adenoma(s) in the rectum are not at increased risk for colorectal
cancer and can be dismissed from follow-up or offered repeat examination at 5 years.
Surgical Resection
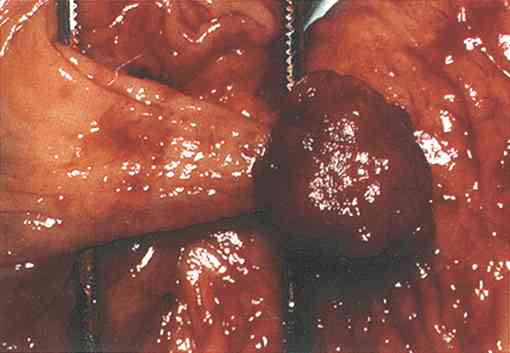
In cases in which a polyp is large and sessile, or otherwise cannot be removed by
endoscopic polypectomy, surgical resection may be necessary. Surgical resection is also
indicated for some adenomas with invasive carcinoma (malignant polyps).Large rectal
adenomas may be extirpated by transanal excision using an operating sigmoidoscope and
rigid snare under anesthesia or with an operating microscope in association with a
sigmoidoscope. Other large polypoid lesions and malignant polyps need to be removed by
laparotomy. Resection of a large villous adenoma of the colon delivered laparoscopically
outside the abdominal wall through a small skin incision is possible. Once laparotomy is
indicated, many surgeons advocate the use of a formal segmental colectomy including lymph
node dissection. The rationale is that when a laparotomy is required for lesions above the
peritoneal reflection, a formal hemicolectomy adds little or no additional anesthesia time
or perioperative mortality and morbidity. The patient's willingness, however, to assume
some risk for potential undertreatment for disease and the patient's ability to maintain
surveillance also are factors that should be considered in any therapeutic decision.
Severe Dysplasia and Intramucosal Carcinoma
These nonmalignant adenomas are cured by adequate polypectomy.
The progression of severe dysplasia to intramucosal car-cinoma and invasive malignancy
demands careful management and complete removal. Evaluation of a removed polyp by
fragmental biopsy or piecemeal polypectomy is diffi-cult. The presence of cancerous cells
on a biopsy or cytology specimen does not reveal the malignant nature of a polyp without
the contextual morphology provided by retrieval of a single specimen in toto. Furthermore,
biopsy may miss an area of invasive carcinoma or be too superficial to make this
diagnosis. Only careful examination of serial sections of the entire polyp after removal
is adequate for proper evaluation. This, of course, is a doctrine of perfection because it
is sometimes impossible to remove a polyp in a single specimen.
Malignant Polyps
When severe dysplasia is noted, careful examination of multiple sections must be done.
When a polyp contains malignant cells that have penetrated the muscularis mucosae, it is
termed a malignant polyp. (see stage)
The proper management of malignant polyps remains controversial. There have
been no prospective trials evaluating the natural history of malignant polyps or their
optimal management strategy. Many features of malignant polyps have been studied for their
predictive potential.
There is general agreement that poor prognostic features include incomplete resection,
poorly differentiated carcinoma, and malignancy present within 2 mm of the polypectomy
margins.More controversial prognostic factors are involvement of venous or lymphatic
channels with malignancy, replacement of the bulk of the adenoma by carcinoma, and large
polyp size. Some studies suggest that the presence of venous or lymphatic invasion is a
grave prognostic factor, and that these patients should undergo colon resection.
Lymphatic invasion is, however, subject to observer variability.Malignant polyps with
venous (or lymphatic) invasion are almost always associated with higher grade cancers,
recurrences, and metastases, but the studies have been mostly retrospective reviews.
Sessile malignant polyps are also considered to have a worse prognosis. In one study, 7 of
34 patients with sessile polyps had local recurrence or distant metastases within 6 years,
compared with none of 47 patients with pedunculated polyps. Again, most of the sessile
polyps usually have other poor risk markers.Of those with pedunculated polyps, most had
invasion limited to the head, neck, or stalk, although one patient had invasion to the
base of the stalk. Of 62 evaluable patients who also had endoscopic polypectomy, 4 had
recurrence (or distant cancer of unknown origin) within 5 years, giving a recurrence rate
of 7%.
In other studies, patients who underwent endoscopic polypectomy for pedunculated malignant
polyps did better. In one study, 19 patients with pedunculated malignant polyps (average
size 3 cm), with one polyp showing venous invasion, were all asymptomatic after 1 to 6
years.In another retrospective review of 43 patients with pedunculated malignant polyps
who were followed for almost 5 years, 19 patients initially underwent colon resection
because of physicians' clinical judgment. Of these 19 patients, as well as the 24 who had
polypectomy alone, none had cancer recurrence. Of the 13 evaluable patients with sessile
polyps, all underwent colon resection, and Dukes B or C cancer was found in. None has had
cancer recurrence after almost 5 years.
Most data indicate that polypoid carcinomas (which have no residual adenomatous tissue) do
not spread and therefore do not require segmental resection unless poor prognostic
features are present.
These guidelines, however, are derived from incomplete studies, and it is difficult to be
rigid in their application. For the individual patient, it is necessary to weigh the
estimated risks of surgery against the risks of leaving residual malignancy in situ after
endoscopic polypectomy of a malignant polyp. The presence of poor prognostic features
should lead the physician to favor colectomy but the decision should always be temporized
by the age of the patient and any coexistent morbidity. The decision depends on an
estimate of the risk that residual cancer is present versus the operative risk if surgery
were undertaken. The latter increases with low rectal lesions, advancing age, and
comorbidity.
Operative mortality ranges from 2% to 10%, increasing with the age of the patient. Because
most patients with malignant polyps are in their seventh and eighth decades of life, the
risk of colectomy is significant. Colectomy would be of little or no benefit if distant
metastases are already present at the time of surgery.
Based on current evidence, the following recommendations for management of malignant
polyps can be made (see
figure)1. A pedunculated malignant polyp with invasion of the head, neck, or
stalk is adequately treated by polypectomy alone if the polypectomy was not piecemeal, the
cancer was not poorly differentiated, and the resection margin was free of cancer for 2
mm.
2. Malignant polyps with involvement within 2 mm of the margin of resection or with
nonassessable margins, polyps with invasion of the submucosa of the bowel wall (especially
if there is less than 2 mm margin of clearance), and polyps containing poorly
differentiated invasive carcinoma should be treated by colectomy unless the surgical risk
is prohibitive. For sessile malignant polyps, invasion of the submucosa of the colonic
wall is present by definition, and surgery should be undertaken, although a 2 mm margin of
clearance can be considered adequate. Blood vessel and lymphatic vessel involvement may
influence a decision to colectomy but not strongly.
3. Malignant polyps treated by polypectomy alone should be followed by colonoscopy within
three months and again at year with biopsy to assess for recurrence at the polypectomy
site. |