Prognostic significance of
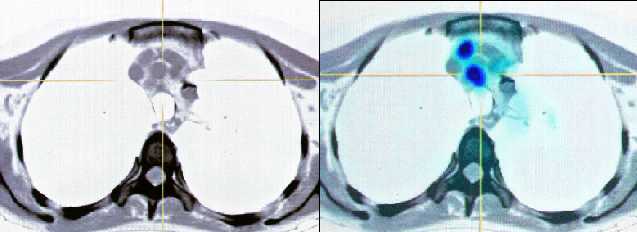
preoperative [18-F] fluorodeoxyglucose (FDG) positron emission tomography
(PET) imaging in patients with resectable soft tissue sarcomas.
Schwarzbach MH, Department of Surgery, University of Heidelberg,
Ann Surg. 2005
Feb;241(2):286-94.
OBJECTIVE: The objective of this study was to evaluate the prognostic
significance of preoperative positron emission tomography (PET) using
2-fluoro-2-deoxy-D-glucose (FDG) by calculating the mean standardized
uptake values (SUV) in patients with resectable soft tissue sarcomas
(STS). In 55 cases, STS were
completely resected: 5-year recurrence-free survival
rates in patients with SUV <1.59, 1.59 to <3.6, and > or =3.6 were 66%,
24%, and 11%, respectively (P = 0.0034).
SUV was a predictor for overall
survival (5-year rates: 84% [SUV <1.59], 45% [SUV 1.59 to <3.6], and 38%
[SUV > or =3.6]; P = 0.057) and local tumor control (5-year rates: 93%
[SUV <1.59], 43% [SUV 1.59 to <3.6], and 15% [SUV > or =3.6]; P =
0.0017).
Intensity of 18Fluorodeoxyglucose
Uptake in Positron Emission Tomography Distinguishes Between Indolent and
Aggressive Non-Hodgkin’s Lymphoma
Heiko Schöder,
JCO Jul 20 2005: 4643–4651.
PET studies of 97 patients with
non-Hodgkin's lymphoma who were untreated or had relapsed
and/or persistent disease and had not received treatment within
the last 6 months were analyzed, and the highest
standardized uptake value (SUV) per
study was recorded. Correlations were made with histopathology.
FDG uptake was lower in
indolent than in aggressive lymphoma for patients with
new (SUV, 7.0 ± 3.1 v 19.6 ± 9.3; P < .01) and relapsed (SUV,
6.3 ± 2.7 v 18.1 ± 10.9; P = .04) disease. Despite overlap
between indolent and aggressive disease in the low SUV range
(indolent, 2.3 to 13.0; aggressive, 3.2 to 43.0), all cases of
indolent lymphoma had an SUV
 13. A receiver operating characteristic (ROC) analysis
demonstrated that the SUV distinguished reasonably well between
aggressive and indolent disease (area under ROC curve, 84.7%),
and an SUV > 10 excluded indolent lymphoma with a specificity
of 81%. With a higher cutoff for the SUV, the specificity would
have been higher.
13. A receiver operating characteristic (ROC) analysis
demonstrated that the SUV distinguished reasonably well between
aggressive and indolent disease (area under ROC curve, 84.7%),
and an SUV > 10 excluded indolent lymphoma with a specificity
of 81%. With a higher cutoff for the SUV, the specificity would
have been higher.
CONCLUSION: FDG uptake is lower in indolent
than in aggressive lymphoma. Patients with NHL and
SUV > 10 have a high likelihood
for aggressive disease. This information may be helpful
if there is discordance between biopsy and clinical behavior. |