INTRODUCTION
In 1307, John of Arderne recorded the several-year evolution of nipple ulceration in a
male priest, with the subsequent development of a breast cancer. In 1840, Velpeau described the visual surface lesion of
Paget's disease in two patients and is typically credited with the first clinical
description of the condition. In 1874, Sir James Paget recorded the association of the
clinical findings with an underlying breast cancer in 15 patients, although he speculated
that the chronic skin condition was benign. It was Thin,
in 1881, who concluded that the clinical Paget's nipple was not a benign
entity, but rather a malignancy. Darier described the microscopic appearance of the
Paget's cell in 1889, although he mistook it for a “psorosperm” or coccidia. In
1928, Pautrier advanced the theory
that the Paget's cell is malignant.
PATHOGENESIS
There are two main theories for the origin of Paget's disease. The epidermotropic
theory, first described by Jacobeus, suggests
that the Paget's cells arise in breast ducts and spread by way of the lactiferous sinuses
to the nipple epidermis. This view is supported by the fact that more than 97% of
patients with Paget's disease have an underlying breast carcinoma and that in the majority of cases, the immunophenotype
of the Paget's cell is the same as the breast cancer.
The intraepidermal transformation theory proposes that the Paget's cells arise in the
terminal portion of the lactiferous duct at its junction with the epidermis; they are
altered epidermal cells that have been transformed in situ. Support for this theory
is found in the rare cases of Paget's disease without an underlying breast carcinoma or cases in which the Paget's disease
and the underlying carcinoma appear to be separate tumors.
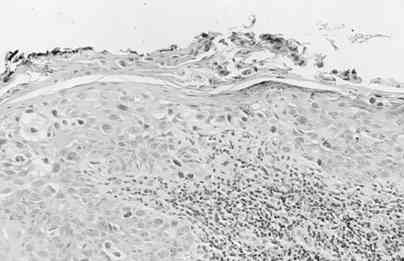
Histologically, the Paget's cell is a large, pale-staining cell with round or oval
nuclei and large nucleoli. The cells are between the normal keratinocytes of the nipple
epidermis, occurring singly in the superficial layers, and in clusters toward the basement
membrane. Serous fluid can seep through the disrupted keratinocyte layer, resulting in the
crusting and scaling of the nipple skin. Paget's cells can traverse the epithelium and
thus sometimes are found in the superficial layers. The basement membrane of the
lactiferous sinuses is in continuity with the basement membrane of the skin. Paget's
cells do not invade through the dermal basement membrane and therefore are a form of
carcinoma in situ. Paget's disease is frequently associated with a chronic
inflammatory infiltrate in the dermis.
CLINICAL PRESENTATION AND
DIAGNOSIS
Paget's disease initially presents with errythema and mild eczematous scaling and
flaking of the nipple skin. Without treatment, the condition advances to crusting, skin
erosion, and ulceration, with exudation or frank discharge. At times, it is associated
with tingling, pruritus, hypersensitivity, burning, or pain. Kister has observed in 117 patients with Paget's disease that
the skin changes always begin on the nipple and secondarily extend to the areola. Given
that the ductal system may connect directly with the areola, Paget's disease may be
confined to the areola, thus mimicking eczema.
The clinical differential diagnosis of scaling skin and erythema of the nipple-areolar
complex includes eczema, contact dermatitis, postradiation dermatitis, and Paget's
disease. Bilateral symptoms are most consistent with eczema or contact dermatitis,
although bilateral Paget's disease has been reported. Skin changes that are confined to
the areola and spare the nipple are typically attributed to eczema, although they can
occur rarely in Paget's disease as well. The clinical differential diagnosis has prompted
initial topical steroid treatment, often with transient improvement of symptoms. Other
patients have been treated with antibiotics. Paget's disease may mimic postradiation
scaling in patients who have undergone breast conservation treatment for primary breast
cancer. Given the infrequency of Paget's disease in this setting, the diagnosis of Paget's
disease may be delayed.Symptom duration preceding the diagnosis of Paget's disease
averages 6.5 to 27.0 months, with a range of 1 week to 20 years.
Less common diagnoses in the clinical differential of mammary Paget's disease include
nipple adenoma, papillomatosis, melanoma,and Bowen's disease, and rarely basal cell
carcinoma, squamous carcinoma, sebaceous carcinoma, Merkel's cell carcinoma, infiltrating
lobular carcinoma, cutaneous T-cell lymphoma, Spitz nevus, epidermatropic metastases,
syringomatous adenoma,pseudoxanthoma elasticum,and pemphigus vulgaris.
The diagnosis can be obtained by scrape cytology, a superficial epidermal shave
biopsy, a 2-mm punch biopsy, a wedge incisional biopsy, or nipple excision. The ideal
specimen contains adequate epidermis to provide Paget's cells and a lactiferous duct.
Paget's cells may be distributed in a patchy fashion throughout the nipple, and thus
additional specimen sampling may be required to secure the diagnosis.
The histologic differential diagnosis of Paget's disease includes superficial spreading
melanoma, squamous cell carcincoma in situ (Bowen's disease), and clear cell
changes of squamous cells of the epidermis (Toker cells). The cell type can be determined
by immunohistochemical studies including low-molecular-weight keratins (CK7, CAM-5.2),
broad-spectum keratins, melanoma antibodies, and mucin stains.
In 807 patients with clinical Paget's disease from 12 series, 371 (46%) presented
with a breast mass, and 436 (54%) presented without a mass. In patients with a
mass, 93% had an invasive breast cancer, and 7% had ductal carcinoma in situ
(DCIS). In patients without a mass, 38% had an invasive breast cancer, and 62% had DCIS.
In Kister and Haagensen's series of
159 patients with histologically confirmed Paget's disease, the mean age of patients with
an associated breast mass was 49 and without a mass 58 (p = .01).
In patients with clinical Paget's disease without a palpable breast mass, mammography
has been reported as normal in 2.5% to 100% of patients.Of the 212 total patients in these
combined series, 91 (43%) had normal mammograms. In seven series, breast histology was
evaluated in those patients with clinical Paget's disease and normal mammograms. All
patients had an underlying malignancy in four of these series (combined n = 44), 12 of 14
(85%) patients had an associated malignancy in the fifth series, 9 of 17 (53%) patients
had an associated malignancy in the sixth series,and four of ten (40%) had an associated
malignancy in the seventh.These retrospective studies included patients accrued in the
late 1970s, when xeromammography was still in use and retroareolar spot compression views
were not routine.
INCIDENCE
Paget's disease is a more common pathologic than clinical entity. Its clinical
incidence ranges from 0.5% to 2.6%, with a mean of 1.1% in more than 44,000 patients
combined from eight studies. Histologic evidence of Paget's cells is present in 0.5% to
4.7% of nipples from breast cancer specimens In a series by Lagios of 3,000
consecutive breast cancer mastectomy specimens, 21 (0.7%) had clinical evidence of Paget's
disease and 147 (4.9%) had Paget's cells histologically, thus yielding a sevenfold
difference.
Of the 158,621 microscopically confirmed female and male breast cancer registrants from
the Surveillance Epidemiology and End Results registry of the National Cancer Institute,
1,775 (1.1%) had histologic Paget's disease. Of breast cancer patients from this database,
Paget's disease was histologically identified in 1.1% of white female patients, 1.3% of
African-American female patients, 1.1% of white male patients, and no African-American
male patients. Clinical Paget's disease has been reported in patients ranging in age from
26 to 88, with means ranging from 53 to 58 years In a further analysis of the Surveillance
Epidemiology and End Results data, the mean age of women with Paget's disease was 62 years
and of men, 69 years. This was not significantly different from female (61 years) and male
(67 years) patients with ductal breast cancer.
TREATMENT
Treatment for Paget's disease has followed the evolution of surgical options for
patients with an invasive breast cancer, with patients with Paget's disease confined to
the nipple-areolar complex now being considered potential candidates for breast
preservation. Physical examination and mammography are used in efforts to identify
multicentric disease and thus the requirement for mastectomy. Identification of a
coexistent invasive breast cancer dictates the role of axillary nodal evaluation.
Breast magnetic resonance imaging (MRI) has shown promise in identifying clinically and
mammographically occult breast cancers. In patients with clinical Paget's disease of the
nipple and physical examination and mammography findings confined to the nipple-areolar
complex, MRI may identify multicentric sites of disease. In this role, it may facilitate
selection of patients in whom breast conservation surgery is not appropriate.
Peripheral breast cancers may not be identified when surgery is limited to excision of
the nipple-areolar complex. In a study of 50 patients with Paget's disease by Paone and
Baker, an underlying cancer was 2 cm or greater from the nipple in 6 (12%) patients, and,
despite multiple microscopic sections, no anatomic connection between the Paget's lesion
and the underlying breast carcinoma could be identified. Ikeda described 11 patients
with clinical Paget's disease without breast masses and with normal mammograms treated
with mastectomy in which DCIS was identified far from the nipple in 6 patients and in two
or more quadrants in 5. Kollmorgen et al.identified 28 patients with Paget's disease and
no breast mass who were found to have an occult tumor on histologic review. One-half of
these were located centrally (within 2 cm of the areolar margin) and one-half
peripherally. Within this group, 17 patients had normal mammograms. Yim described 11
patients with clinical Paget's disease, no palpable mass, and pathologically confirmed
multifocal disease. In these 11 patients, mammography identified multifocal disease in 4
(36%) patients and failed to identify multifocal DCIS in 7 (64%) patients, 2 of whom also
had mammographically occult invasive ductal carcinoma in noncentral breast quadrants. In
an analysis of 100 consecutive mastectomy specimens, Wertheim and Ozzello identified 18 cases of Paget's disease, 4 (22%) of which
had invasive cancers in peripheral quadrants of the breast.
Breast Conservation without
Radiation
Failure to identify peripheral cancers when patients are treated with breast
conservation surgery without irradiation may yield increased local failure rates. In a
series reported by Dixon ten patients with Paget's disease without an associated
mass and with negative mammographic findings or findings suggestive of in situ
changes confined to the immediate nipple area underwent excision of the nipple-areolar
complex with underlying cone biopsy. All ten specimens had underlying DCIS, one had an
associated invasive breast cancer, and all had negative surgical margins. With a median
follow-up of 40 months, there were four local recurrences, one as Paget's in the surgical
scar and the other three as invasive cancers. Metastatic disease subsequently developed in
two patients. Dixon et al. conclude by advocating simple mastectomy for treatment of
patients with clinical Paget's disease even in the absence of an associated breast mass.
In contrast, Paone and Baker
described five patients with Paget's disease without an associated breast mass treated
with nipple excision and underlying breast wedge resection. Although there were no
recurrences, the length of follow-up is not specified. Lagios reported on five
patients with clinical Paget's disease without an associated palpable mass or mammographic
abnormality. Treatment involved breast conservation surgery alone. Of the four patients
undergoing total excision of the nipple-areolar complex, no recurrences were seen at 16 to
55 months (median, 36 months) after treatment. In the patient who underwent partial
resection, the remainder of the nipple-areolar complex was resected at the time of
recurrence 12 months after the initial resection. The patient has no evidence of further
recurrence at 43 months. Detailed pathologic review of these five specimens demonstrated in
situ disease confined to the protuberant nipple in two patients and DCIS to a depth
not exceeding 8 mm in three patients. A sixth patient had undergone mastectomy, and a
single involved lactiferous duct was identified to a depth of 15 mm.
Breast Conservation with Radiation
The addition of radiotherapy (XRT) may add to the efficacy of breast-conserving surgery
for patients with Paget's disease. In an abstract from Memorial Sloan-Kettering Cancer
Center, 14 patients with clinical Paget's disease without evidence of invasion underwent
central quadrantectomy achieving negative surgical margins. Of the nine patients who
received XRT (6,120 cGy), one had a recurrence. Of the five patients not receiving XRT,
three had recurrences. Time to recurrence was not specified.
Pierce present 30 patients with Paget's disease without a palpable mass or mammographic
density from seven institutions. All patients were treated with breast irradiation with
varying extents of surgical excision. Mammography review was available for 29 patients; in
24, it was negative; in 3, it demonstrated nipple thickening; in 2, retroareolar
calcifications; and in 1, calcifications elsewhere in the breast. Twenty-two patients
underwent complete excision of the nipple (3) or nipple-areolar (19) complex, 6 underwent
partial excision of the nipple (4) or nipple-areolar (2) complex, and 2 patients underwent
incisional biopsy only for histologic confirmation of Paget's disease. All patients
received whole breast irradiation to a median dose of 50 Gy, with 97% receiving a boost to
the tumor bed for a median total dose of 61.5 Gy. With median follow-up of 62 months, five
inbreast recurrences were detected, three (14%) in the group treated with complete
excision of the nipple or nipple-areolar complex and two (33%) in the group treated with
partial excision. Additionally, one patient had an ipsilateral axillary recurrence in 6 of
19 involved lymph nodes, and another patient had a contralateral axillary occurrence. Two
patients are alive with distant disease, one patient having a local failure first and the
other having the contralateral axillary occurrence (L. J. Pierce, personal
communication, 14 January 1999). Pierce concludes that breast-conserving therapy
involving complete nipple-areolar excision followed by XRT should be considered in
patients with localized Paget's disease, given the adequate local control and high rates
of disease-free survival. The efficacy of central quadrantectomy and XRT (50 Gy) in
patients with Paget's disease and DCIS limited to the retroareolar ducts will be further
defined in the ongoing nonrandomized study of 100 patients by the European Organization
for Research and Treatment of Cancer.
Radiation without Surgery
The possibility of radiation treatment alone for patients with Paget's disease without
a palpable mass or abnormal mammogram has been reported. In a photographic case report by
Hareyama a patient with advanced Paget's disease involving the entire nipple-areolar
complex was treated with whole-breast irradiation to 5,400 cGy. At 6 years posttreatment,
she is without evidence of recurrence and has an excellent cosmetic result. El Sharkawi
and Waters provide a similar photographic essay in three patients 3 to 5 years after
treatment with XRT of 3,500 to 4,500 cGy focused to the nipple-areolar region alone.
presents four reports of patients with histologically confirmed Paget's disease
without evidence of invasion and treated with irradiation alone.
At a median follow-up of 63 to 90 months after treatment, 10 of the 63 patients (16%)
developed inbreast recurrences, 6 as Paget's disease, 2 as microinvasive DCIS, and 2
as invasive breast cancer. The patient with an invasive recurrence died of metastatic
disease 9.5 years after initial treatment.
Axillary Dissection
The indication for axillary dissection in the patient with clinical Paget's disease
without other physical examination or radiologic findings is not well defined. In 15
combined series of patients with clinical Paget's disease without a palpable mass,
axillary metastases were identified in 50 of 417 (12%) patients (range, 0 to 25%).
These studies were predominantly from the premammography era. Kollmorgen recommends axillary dissection in all patients with
Paget's disease. In his series of 68 patients with clinical Paget's disease, a subset of
32 without a palpable mass underwent axillary dissection, with nodal positivity identified
in 6 patients (19%). Neither the mammography findings of this patient subset nor whether
these six patients had a concurrent invasive breast cancer is specified.
MANAGEMENT SUMMARY
The diagnosis of Paget's disease is confirmed by nipple scrape cytology or biopsy.
Retroareolar spot compression views of the ipsilateral breast should be added to
standard bilateral mammography. If available, preoperative breast MRI can be obtained to
evaluate for possible occult disease in patients who are considering breast preservation. Patients
with disease identified beyond the central portion of the breast by physical examination
or breast imaging studies should undergo mastectomy. For patients choosing breast
conservation therapy, strong consideration should be given to combining surgery and
radiation in efforts to minimize future local recurrence. For patients undergoing
either mastectomy or breast conservation, the decision for axillary node dissection should
be based on the presence of an invasive breast cancer. Adjuvant therapy decisions are
based on the final pathology.
Patients with clinical and mammographic disease limited to the retroareolar area can
be considered candidates for breast conservation. Surgery should include excision of the
full nipple-areolar complex with at least a 2-cm cone of retroareolar tissue and complete
excision of abnormal retroareolar radiologic findings. For patients with positive margins
after central quadrantectomy, consideration for mastectomy should be given. Patients with
negative surgical margins should undergo irradiation. |