The role of fluorodeoxyglucose
positron emission tomography in cervical lymph node metastases from an unknown primary
tumor
Kyle E. Rusthoven, Mary Koshy, Arnold C. Paulino Cancer 2004;101:2641
The overall sensitivity, specificity,
and accuracy rates of FDG-PET in detecting unknown primary tumors were 88.3%, 74.9%, and
78.8%, respectively. Furthermore, FDG-PET detected 24.5% of tumors that were not apparent
after conventional workup. FDG-PET imaging also led to the detection of previously
unrecognized metastases in 27.1% of patients (regional, 15.9%; distant, 11.2%). FDG-PET
had notably low specificity and a high false-positive rate (39.3%) in the tonsils. In
contrast, the false-positive rates for FDG-PET of the base of tongue and hypopharynx were
only 21.4% and 8.3%, respectively. FDG-PET exhibited decreased sensitivity to tumors in
the base of tongue (81.5%). The sensitivity of this technique at other sites was 90.5%.
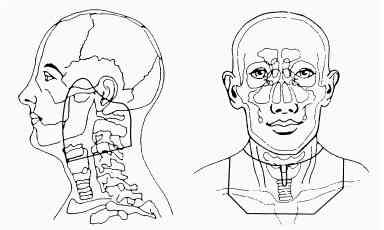
The detection of primary tumors in patients with
cervical lymph node metastases is important for several reasons, including target volume
delineation and treatment-associated morbidity. Patients with known primaries in the head
and neck receive site-specific treatment, whereas patients with persistent unknown
primaries after conventional workup often undergo irradiation of mucosal sites, where
primary tumors commonly occur. The mucosal sites that undergo elective irradiation vary
according to distribution of involved lymph nodes but commonly include the nasopharynx,
base of tongue, and hypopharynx. Because of the larger target volume involved, such
panmucosal radiotherapy can cause additional morbidity when compared with the radiotherapy
administered to treat a known primary tumor.
The rate of primary tumor detection by FDG-PET in
the current series was slightly improved relative to the rate reported in the review by
Fogarty Those investigators found that FDG-PET correctly detected a primary tumor
that had gone undetected by CT/MRI in 62 of 276 cases (22.5%). Our analysis suggests that
FDG-PET provided additional information beyond conventional anatomic imaging in 24.5% of
patients. More impressive was the difference in specificity between the current review
(74.9%) and the reviews conducted by Fogarty et al. (65.3%) and Neider et al. (62%). The
lower false-positive rate in the current series was attributable in part to the exclusion
of data from FDG-SPECT. In addition, our analysis includes data from 4 studies and 125
patients who were not included in those previous reviews. The specificity of FDG-PET in
these 4 studies was 74%, which is consistent with the data from the rest of our analysis.
Despite this improvement, however, low specificity remains the most notable weakness of
FDG-PET. Proposed reasons for the high false-positive rate include physiologic uptake in
the tonsils, reactive lymph nodes, and muscles of mastication. Less commonly, FDG
accumulation can occur in patients with sarcoidosis, granulomatous disease, and benign
tumors of the salivary glands. Stokkel have also suggested that recent mucosal
biopsy in the workup of unknown primaries can cause a tissue repair reaction with a
consequent increase in FDG uptake. Finally, Greven suggested that the high
false-positive rate also may be attributable to sampling error in PET-directed biopsies.
In the current series, FDG-PET exhibited high
sensitivity (88%) in the detection of primary tumors. Neider et al. reported a slightly
lower sensitivity for this technique (82%). Kole have suggested several possible causes
for false-negative results; disruption of the signal-to-noise ratio caused by high
background uptake, especially in the brain, can disrupt the detection of a tumor, and in
addition, well differentiated tumors have been shown to have a lower rate of FDG uptake.
Kole and colleagues have also suggested that small tumors that are below the resolution of
FDG-PET can lead to false-negative results. Nonetheless, the high sensitivity of FDG-PET
in the current review can be attributed to the large number of true-negative results. In
our analysis, 61.9% of patients (187 of 302) never had a primary tumor found, and FDG-PET
yielded true-negative findings in 46.4% of all patients (140 of 302 patients). Some have
speculated that the failure to detect a primary tumor after extensive workup may be the
result of phenomena such as spontaneous regression or immune-mediated destruction of the
primary lesion.
The most notable utility of FDG-PET imaging was
its ability to detect new metastases. Three of the four studies that reported information
on the detection of new metastases used whole-body FDG-PET. In the study by Fogarty
all three sites at which new distant metastases were found were located below the
diaphragm. Braams et also comment on the possibility that both primary tumors and distant
metastases could localize below the clavicle and advise that whole-body FDG-PET be used,
especially when the metastases are located in the lower part of the neck. Overall, the
data from the current review indicated that whole-body imaging was able to detect
unsuspected regional or distant disease in 27% of all patients.
The detection of unknown distant metastases
occurred in 11% of all patients reviewed. This finding is particularly important, because
such information can lead to a change in the treatment objective from cure to palliation.
Moreover, previously unrecognized regional disease, the detection of which could lead to
inclusion of the contralateral neck in target delineation or to the administration of a
higher radiotherapy dose to FDG-PET-positive lymph node sites, was found in 16% of
patients. In the current review, data from FDG-PET scans led to changes in treatment in
24.7% of all patients in the 6 studies in which this endpoint was reported.
Our findings regarding primary tumor locations are
consistent with those made in previous studies. In the current study, 24% of all primary
tumors in patients with cervical lymph node metastases and unknown primaries were found
below the clavicle. In their report, Jones found that up to 40% of patients with
malignant cervical lymph nodes had primary tumors outside of the head and neck (most
commonly in the lungs). Among head and neck primaries, tumors of
the tonsils and the base of the tongue were the most prevalent in the current
analysis. Similarly, in the study by Mendenhall tumors of the tonsils and the base
of the tongue accounted for 43% and 39% of all primary tumors, respectively. Data from the
current series also suggest a lower incidence of primary tumors of the nasopharynx (8.3%),
hypopharynx (8.3%), and supraglottic larynx (5.3%) than has been previously reported in
the literature on CUP.Mendenhall suggest that the decreased incidence of unknown tumors at
these locations can, in all likelihood, be attributed to the increased sensitivity of
fiberoptic endoscopes and anatomic imaging (CT/MRI) in the detection of primary tumors at
these sites. In contrast, tumors of the tonsils and base of tongue can resemble lymphoid
tissue and thus can be more difficult to detect with conventional workup.
In our audit, FDG-PET exhibited its highest
accuracy for tumors of the hypopharynx and larynx. The high sensitivity (100%) and low
false-positive rates (10%) that were observed indicate that FDG-PET is a valuable
supplement to panendoscopy at these locations.
The most common site of false-negative FDG-PET
findings in the current analysis was the base of tongue (sensitivity, 79.3%). The observed
reduction in sensitivity can be attributed to the high baseline level of FDG uptake (as a
result of speech and swallowing) at this site.[33]
Consequently, FDG uptake by a tumor located at the base of the tongue can be
misinterpreted as benign physiologic uptake. Because of the high false-negative rate, it
is recommended that patients with negative FDG-PET findings at this site undergo further
investigation, including panendoscopy and biopsy.
FDG-PET had a low false-positive rate for tumors
located at the base of the tongue or in the hypopharynx. In the current series, there were
only six false-positive diagnoses of tumors at the base of the tongue and only one
false-positive diagnosis of a tumor in the hypopharynx. The low false-positive rate that
was observed corresponds to a high specificity and positive predictive value for FDG-PET
detection of tumors at these sites.
At anatomic locations other than the base of the
tongue and the hypopharynx, false-positive rates were much higher. The tonsils were the
most common site of false-positive FDG uptake (39.3%, compared with 28.3% for all other
sites combined). The high rate of false-positive results and the low specificity of
FDG-PET for tonsillar tumors can be attributed to FDG uptake caused by increased cellular
metabolism in inflammatory lesions. Li found that inflammatory lesions had a mean
FDG standardized uptake value (SUV) of 2.58 (standard deviation, 0.77). Similarly, Adams
et al.[37]
found that inflamed lymphoid tissue had SUV values that ranged from 2.0 to 15.8. This
enhanced FDG uptake by benign lesions in the tonsils overlaps with the range of uptake
levels found in malignancies and can, therefore, lead to false-positive results.
False-positive FDG-PET findings subject the patient to further diagnostic investigation
and mucosal biopsy, which have associated costs and morbidities.
CONCLUSIONSFDG-PET detected primary tumors that went undetected by other modalities in
approximately 25% of cases and was sensitive in the detection of previously unrecognized
regional or distant metastases in 27% of cases. FDG-PET had low specificity for tonsillar
tumors and low sensitivity for base-of-tongue malignancies
|