|
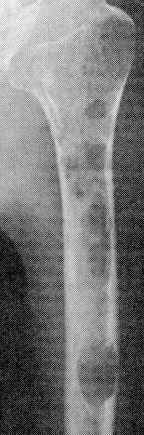
Multiple Myeloma Bone Disease
for images go
here and
radiation go here Bone pain, particularly in the back or chest, and less often in the extremities, is present at the time of diagnosis in approximately 60 percent of patients. The pain is usually induced by movement and does not occur at night except with change of position. The patient's height may be reduced by several inches because of vertebral collapse. Conventional radiographs reveal an
abnormality in approximately 80 percent of patients at the time of
diagnosis. Focal lytic lesions are found in nearly 60 percent; osteoporosis,
pathologic fractures, or compression fractures of the spine each occur in
approximately 20 percent of patients. Hypercalcemia is found in 28 percent;
serum calcium is Mechanisms — Bone resorption in multiple myeloma is accelerated due to increases in both the proportion of the bone interface undergoing resorption and the amount of bone resorbed within individual areas; the latter effect is due to an increase in the number and activity of osteoclasts within these sites. Development of osteolytic lesions appears to occur through at least two different mechanisms, via the production of various cytokines by myeloma cells adjacent to bone
Imaging — A number of modalities are available for the imaging of bone lesions. The most useful modalities for patients with myeloma include routine skeletal surveys (metastatic bone surveys) and MRI. Skeletal surveys — Conventional skeletal surveys reveal punched-out lytic lesions diffuse osteopenia, or fractures in nearly 80 percent of patients with multiple myeloma at the time of diagnosis. The vertebral bodies, skull, thoracic cage, pelvis, and proximal humeri and femora are the most frequent sites of involvement. Osteosclerotic lesions are rare CT and MRI — Computed tomography and magnetic resonance imaging (MRI) are especially helpful in patients who have bone pain but no abnormalities on routine roentgenograms MRI may also be of prognostic value in determining which patient with low cell mass myeloma is most likely to progress As an example, in 55 asymptomatic patients with stage I myeloma and negative skeletal surveys, disease progression was noted in 47 versus 5 percent of patients with abnormal or normal spinal MRI patterns, respectively In the absence of osteopenia or focal osteolytic lesions on standard metastatic bone surveys, MRI can detect diffuse and focal bone marrow lesions in patients with myeloma. However, the two modalities may be complementary. In one study in which 611 patients with myeloma had both MRI imaging (limited to the axial bone marrow) as well as a standard metastatic bone survey, MRI detected focal lesions in 52 percent of those with negative bone surveys, while bone surveys detected focal lesions in 20 percent of those with a negative MRI . Significantly higher proportions of patients had focal lesions detected on MRI in the spine, pelvis, and sternum, while bone surveys outperformed MRI for lesions in the ribs and long bones. Bone scanning — Technetium-99m bone scanning (which primarily detects osteoblastic activity) is inferior to conventional roentgenography for the detection of lytic lesions and should not be used [ PET scanning — Experience with PET scanning in patients with multiple myeloma using fluorine-18-labeled FDG is limited. In one small series, PET scanning detected some lesions missed by other techniques; however, false positive as well as false negative results were also reported. Until further information is available on the accuracy of PET scanning in myeloma, such scans should be performed only in a study or protocol setting.
|