J Am Dent Assoc 1985 Jul;111(1):49-54
Prevention of
osteoradionecrosis: a randomized prospective clinical trial of hyperbaric oxygen versus
penicillin.
Marx RE, Johnson RP, Kline SN
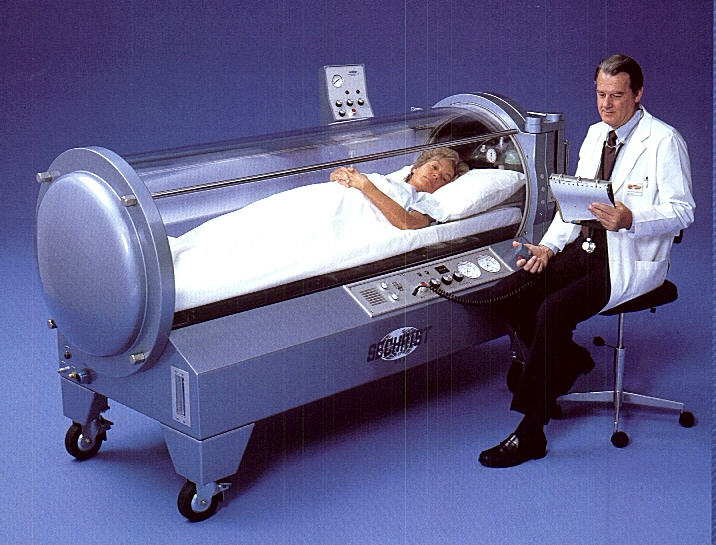
A prospective randomized trial comparing hyperbaric oxygen and systemic antibiotics in
the prevention of osteoradionecrosis was presented. The results indicated, in a high-risk
population who required tooth removal in irradiated mandibles, that up-front hyperbaric
oxygen produced an incidence of osteoradionecrosis of 5.4% as compared with the antibiotic
group of 29.9% (P = .005). Hyperbaric oxygen should be considered a prophylactic measure
when post-irradiation dental care involving trauma to tissue is necessary.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995 Jul;80(1):12-6
Hyperbaric oxygen treatment of osteoradionecrosis of the mandible. Experience
in 29 patients.
van Merkesteyn JP, Bakker DJ, Borgmeijer-Hoelen AM
Department of Oral and Maxillofacial Surgery, Academic Hospital Leiden, The
Netherlands.
In recent years hyperbaric oxygen has gained an important role in the treatment of
osteoradionecrosis of the mandible. In the treatment of 29 patients with
osteoradionecrosis of the mandible, a combination of surgical debridement, antibiotics,
and hyperbaric oxygen was used in 27 cases. In 20 of the 29 patients the
osteoradionecrosis was considered to be resolved after treatment. In 31% of the patients,
the continuity of the mandible was lost. It was concluded that combined treatment of
surgical debridement, antibiotics, and hyperbaric oxygen gives acceptable results and may,
when used in an early phase of the disease, limit the number of patients who lose
continuity of the mandible.
Br J Oral Maxillofac Surg 1996 Oct;34(5):424-7
Does hyperbaric oxygen have a role in the management of osteoradionecrosis?
Wood GA, Liggins SJ
Department of Oral and Maxillofacial Surgery, Canniesburn Hospital, Bearsden, Glasgow,
UK.
A retrospective study of 12 episodes of osteoradionecrosis treated with hyperbaric
oxygen (HBO) in 11 patients was carried out. The cases had been previously treated by more
conventional methods including surgery, unsuccessfully. All the cases treated by HBO had a
successful outcome, although 83% of the patients required concomitant surgery to remove
necrotic bone. The costs and contra-indications for hyperbaric oxygen therapy are
discussed.
Aust Dent J 1999 Dec;44(4):243-7
Hyperbaric oxygen in the prevention of osteoradionecrosis of the jaws.
Vudiniabola S, Pirone C, Williamson J, Goss AN
Oral and Maxillofacial Surgery Unit, University of Adelaide.
Patients who have had their jaws irradiated as part of management of head and neck
malignancy are at risk of osteoradionecrosis (ORN) following tooth extraction.
Thirty-seven patients with a history of irradiation to the jaws were managed during a four
year period. Twenty-nine patients received hyperbaric oxygen therapy (HBO) consisting of
20 treatments before surgery and ten treatments after. Only one (4 per cent) developed
ORN. Seven patients who did not have HBO and one who did (15 per cent) developed ORN. The
need for prophylactic treatment with HBO is discussed. It is recommended that prophylactic
HBO is used prior to surgery for irradiated facial bones.
Laryngoscope 1993 Jun;103(6):605-8
Role of hyperbaric oxygen therapy in the management of mandibular
osteoradionecrosis.
Mounsey RA, Brown DH, O'Dwyer TP, Gullane PJ, Koch GH
Department of Otolaryngology, Toronto Hospital, Ontario, Canada.
Hyperbaric oxygen (HBO) has been used as a tool in the management of osteoradionecrosis
(ORN). However, it has not been conclusively proven to be of benefit. The precise role and
guidelines for its use also have not been clearly defined. This report retrospectively
analyzes 41 patients treated at the Hyperbaric Chamber Unit at the Toronto Hospital
(Toronto General Division) with proven mandibular ORN from 1980 to 1985. The results show
that 83% of the patients had a significant improvement with HBO therapy, judged by at
least a 50% decrease in the size of the exposed bone, closing of the fistulous tract, or
complete relief of symptoms. Within the group of patients who were significantly improved,
15% showed complete resolution of ORN. Seven (17%) of the patients did not benefit from
the HBO. All seven patients had radiological evidence of dead bone. Based on these
observations, the following conclusions can be made: 1. HBO is of benefit in the
management of ORN. 2. Patients with ORN may be divided into two groups: mild and severe.
3. Cases of mild ORN will heal with HBO alone, but, in severe ORN, surgery is necessary to
remove dead bone. 4. All patients with ORN should receive dental evaluation, local wound
care, and a strict oral hygiene regimen. Diseased teeth should be removed prior to
radiotherapy. Subsequently, any teeth that became abscessed should be extracted in
conjunction with prophylactic HBO. Antibiotics play an ancillary role in the management of
ORN. For patients who have received radiation to the mandible, the authors propose regular
follow-up in order to detect ORN at a time when HBO can arrest the disease.
Oral Surg Oral Med Oral Pathol 1987 Mar;63(3):280-6
Hyperbaric oxygen in the treatment of osteoradionecrosis: a review of its use
and efficacy.
Fattore L, Strauss RA
Hyperbaric oxygen (HBO) therapy is an established technology that is proving to be
effective in the treatment of osteoradionecrosis. However, the studies that have shown
this treatment modality to be effective have not established the optimum pressures, times
of exposure, and frequency and number of treatment necessary for healing. In addition,
most of the studies used HBO as an adjunctive treatment in the management of refractory
osteoradionecrosis. The efficacy of HBO as a primary treatment modality has not as yet
been established. Strictly controlled clinical trials are necessary for identification of
patients who are likely to respond to HBO without aggressive surgery, to delineate a
timetable for treatment of patients with HBO, and to coordinate surgery with HBO to
resolve osteoradionecrosis when a significant amount of bone loss is involved.
SADJ 1998 Oct;53(10):469-71
A review of the Marx protocols: prevention and management of osteoradionecrosis
by combining surgery and hyperbaric oxygen therapy.
Cronje FJ
Institute for Aviation Medicine, Hyperbaric Oxygen Therapy Department, Pretoria.
The 30/10 protocol is employed in the treatment of established osteoradionecrosis. No
surgery should be attempted before the first 30 HBO treatments have provided sufficient
angiogenesis to support surgical wounding. After 30 treatments surgical management can be
staged according to the extent of improvement achieved after HBO and the size of
sequestrum or area of osteolysis. If the ORN extends to the inferior border of the
mandible or if it manifests as an orocutaneous fistula or pathological fracture,
discontinuity resection of the necrotic bone and soft tissue will be required to resolve
the disease. Unless HBO and surgery are combined in the management of ORN, the results are
not long lasting or satisfactory. Even though resection of stage three ORN seems unduly
aggressive, it has stood the test of time. By using the Marx protocols in the treatment of
ORN, more than 95 per cent of patients can be successfully cured of their disease with
predictable, functional and aesthetically acceptable outcomes. |