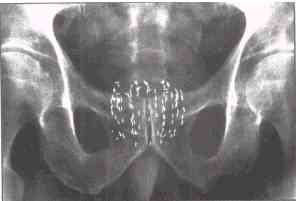
Combined modality treatment in the management of high-risk prostate
cancer (see graph above)
Between February 1994 and November 1999, 132 high-risk patients were treated with combined
hormonal therapy (9 months), permanent radioactive seed brachytherapy, and external
beam RT, with follow-up ranging from 36 to 88 months (median, 50 months). The
eligibility criteria were any of the following: Gleason score 8–10, initial
prostate-specific antigen (PSA) level >20 ng/mL, clinical Stage T2c-T3, or positive
seminal vesicle biopsy, or two or more of the following: Gleason score 7, PSA level
>10–20 ng/mL, or Stage T2b. Twenty percent of patients had a positive seminal
vesicle biopsy before therapy. Negative laparoscopic pelvic lymph node dissections were
performed in 44% of patients.
Results: The actuarial overall freedom from PSA failure rate was 86% at 5 years. The
freedom from PSA failure rate at 5 years was 97% for those with a Gleason score of ?6 (35
of 36), 85% for a Gleason score of 7 (50 of 59), and 76% for a Gleason score of 8–10
(28 of 37; p = 0.03). A trend was noted toward worse outcomes in seminal vesicle
biopsy-positive patients, with a 5-year freedom from PSA failure rate of 74% vs. 89% for
all other patients (p = 0.06). Posttreatment prostate biopsies were performed in 47
patients and were negative in 96% at the first biopsy and 100% at the last biopsy.
Conclusion:Trimodality therapy with androgen suppression, brachytherapy, and external beam
RT for high-risk prostate cancer results in excellent biochemical and pathologically
confirmed local control.
Mol Urol 2000 Autumn;4(3):163-8
Effects of neoadjuvant hormonal therapy on prostate biopsy results after (125)I and
(103) Pd seed implantation
Stone NN, Stock RG, Unger P
Departments of Urology and Radiation Oncology, Mount Sinai School of Medicine, New
York, New York.
A total of 296 patients who had either (125)I (206; 70%) or (103)Pd (90; 30%)
transperineal prostate brachytherapy (no external-beam radiation) had routine transrectal
ultrasound-guided needle biopsy (minimum six cores) 2 years after treatment without regard
to disease status. Neoadjuvant hormonal therapy (NHT: leuprolide acetate and flutamide)
was used in 115 patients (39%) for 3 months prior to and 3 months after the implant.
Results: Of the 296 patients, 30 (10%) had positive prostate biopsies. Biopsies were
positive in 4 of 115 (3.5%) v 26 of 181 (14%) of those who received or had not received
NHT, respectively (P = 0.002). When patients were separated into
low risk (PSA </=10 ng/mL, stage </=T(2a), and Gleason score </= 6) and high risk
(all others), it was seen that low-risk patients did not benefit from NHT (3.8 v 7.7%
positive biopsy rate; P = 0.5) whereas high-risk patients did (3.4% v 21.1%; P = 0.003).
Mol Urol 1999;3(3):239-244
Neoadjuvant Hormonal Therapy Improves the Outcomes of Patients Undergoing Radioactive
Seed Implantation for Localized Prostate Cancer.
Stone NN, Stock RG
Department of Urology, Mount Sinai Medical Center, New York, New York.
In this report, we describe the effects of NHT on prostate volume (PV) prior to seed
implantation and on the prostate specific antigen (PSA) and postimplant biopsy outcomes of
patients who presented with high-risk features. Hormone therapy (leuprolide and flutamide
750 mg/day) was given to 145 patients for
3 months prior to and for 3 months
after permanent iodine-125 (160 Gy) or palladium-103 (115 Gy) seed
implantation. Prostate volume was measured in 106 patients
prior to NHT and 3 months later immediately prior to the seed implant. The mean PV was
50.4 cc (range 17-150 cc), whereas the mean PV after NHT was 31 cc (range 11.7-73.7
cc). The mean PV reduction was 35% (range 2%-62%). Volume reduction was compared in
those patients who presented with a PV <40 cc (N = 51) and those
with a PV >/=40 cc (N = 56). The mean reduction for the smaller glands was 29% (range
2%-54%) compared with 41% (range 7%-62%) for the larger glands (P < 0.05).
Patients were followed for a minimum of 1 year (range 1.0-6.4; mean 2.2 years). |