| Treatment and Prognosis of Squamous Cell
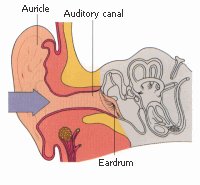
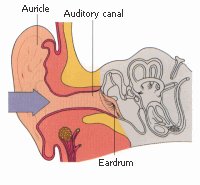
Carcinoma of the External
Auditory
Canal and Middle Ear: A
Multi-Institutional Retrospective Review of 87 Patients
Ogama IJROBP 2007;68:1326
Purpose: To examine the relative roles of surgery, radiotherapy, and
chemotherapy in the management of patients with squamous cell carcinomas of
the external
auditory
canal and middle ear.
Methods and Materials:
The records of 87 patients with histologically confirmed squamous cell
carcinoma who were treated between 1984 and 2005 were reviewed. Fifty-three
patients (61%) were treated with surgery and radiotherapy (S + RT group) and
the remaining 34 patients with radiotherapy alone (RT group). Chemotherapy
was administered in 34 patients (39%).
Results: The 5-year
actuarial overall and disease-free survival (DFS) rates for all patients
were 55% and 54%, respectively. On univariate analysis, T stage (Stells
classification), treatment modality, and Karnofsky performance status had
significant impact on DFS. On multivariate analysis, T stage and treatment
modality were significant prognostic factors. Chemotherapy did not influence
DFS. The 5-year DFS rate in T1, T2,
and T3 patients was 83%, 45%, and 0 in the RT group (p < 0.0001) and 75%,
75%, and 46% in the S + RT group (p = 0.13), respectively. The 5-year
DFS rate in patients with negative surgical margins, those with positive
margins, and those with macroscopic residual disease was 83%, 55%, and 38%,
respectively (p = 0.007).
Conclusions:
Radical radiotherapy is the
treatment of choice for early-stage (T1) diseases, whereas surgery
(negative surgical margins if possible) with radiotherapy is recommended as
the standard care for advanced (T23) disease. Further clarification on the
role of chemotherapy is necessary.
Treatment Outcomes of Squamous Cell Carcinoma of
External
Auditory
Canal and Middle Ear
Yoshida. IJROBP 2009;675:S424
The occurrence of squamous cell carcinoma (SCC) of
external
auditory
canal (EAC) and middle ear is
extremely rare with a yearly incidence of around 1 per 1 million people.
Because of the rarity of this entity, there are few retrospective and no
prospective studies. The purpose of this study is to evaluate our treatment
outcomes of SCC of EAC and middle ear.
Between 1990 and 2008, 38 patients with SCC of EAC and middle ear treated
at our institute were retrospectively investigated. Twenty-nine (76%)
patients had primary EAC cancer and 9 (24%) had primary middle ear cancer.
There were 15 (39%) males and 23 (61%) females. Fourteen (37%) patients had
T12 disease and 24 (63%) had T34 disease according to the Pittsburgh
classification. Lymph node involvement was found in 7 (18%) patients.
Thirteen (34%) patients received surgery (S), 12 (32%) received radiotherapy
(RT), and 13 (34%) received surgery combined with radiotherapy (S + RT). All
14 patients with T12 disease received S with or without RT. All 12 patients
of RT group had T34 disease and 9 (75%) of them received concurrent
chemoradiotherapy. The median total radiation dose of 25 patients treated by
RT was 60 Gy (range, 2470 Gy). The median overall treatment time for RT was
41 days (range, 1554 days).
The median follow-up period was 32 months (range, 1122 months). There
were 10 patients who experienced recurrence. Six had local, 3 had local and
regional lymph node, and 1 had regional lymph node recurrence. Twelve
patients died during the period of this study. Ten died of primary disease
(including postoperative epidural hematoma) and 2 died of other causes (contralateral
palotid gland cancer and acute myocardial infarction). The 5-year overall
survival (OS), disease-specific survival (DSS), and locoregional control (LRC)
rates for all patients by Kaplan-Meier method were 66, 72, and 69%,
respectively. The 5-year OS, DSS, and LRC rates according to treatment
modality (S/RT/S + RT) were 77/53/63% (p = 0.49 by log rank test), 84/53/63%
(p = 0.51), and 83/53/66% (p = 0.56), respectively.
The 5-year OS, DSS, and LRC rates according to T-Stage (T12/T34) were
92/50% (p = 0.03), 92/52% (p = 0.02), and 85/57% (p = 0.11), respectively.
No patient had Grade 3 or greater acute radiation toxicity. One patient of S
+ RT group had Grade 4 osteonecrosis as late radiation toxicity.
Conclusions
Our treatment outcomes of T12 disease were excellent and those of T34
disease were compatible with several previous reports. Although the standard
treatment modalities of SCC of EAC and middle ear is still unclear because
of the rarity, our results indicate that S with or without RT are
recommendable for T12 disease and concurrent chemoradiotherapy may be a
useful modality for T34 disease.
Squamous Cell Carcinoma of the
External
Auditory
Canal: Long-term Clinical
Outcomes at the University of Florida
Prabhu IJROBP
Squamous cell carcinoma of the
external auditory
canal (EAC) is a rare diagnosis
for which radiotherapy often plays an important role in local control. This
retrospective review describes the University of Florida's 27-year
experience treating these tumors.Thirty patients with histologically
confirmed squamous cell carcinoma of the EAC were treated between 1976 and
2003 at our institution. Seven patients were treated with definitive
radiotherapy (RT), 22 patients with postoperative adjuvant RT, and 1 patient
with preoperative RT. Patients were grouped according to nodal status
(N0/N1) and Stell's staging system for tumors of the EAC and middle ear.
Early stage was defined as T1/T2 (n = 12) and late stage was defined as T3
(n = 18). Median follow-up was 2 years (range, 0.1-19.4 years) with no
patients lost to follow-up.
The 5-year actuarial local
control, local-regional control, and cause-specific survival rates for
patients with early-Stage (T1/T2) vs. late-Stage (T3) tumors were 74% vs.
55% (p = 0.27), 63% vs. 38% (p = 0.16), and 70% vs. 41% (p = 0.04),
respectively. The overall local control, local-regional control, and
cause-specific survival rates were 62%, 48%, and 54%, respectively. The
regional control rate was 83% (p = 0.6) for both the clinical N0 and N1
groups. There were 12 local recurrences and 4 neck recurrences as the first
site of failure with 1 successful surgical salvage. Five of 24 (21%)
patients who underwent surgery had significant complications (Grade 3 or 4)
while 2 of 30 (7%) patients who underwent RT had Grade 3 complications.
Conclusions
This study represents one of the largest series specifically addressing
outcomes following RT for squamous cell carcinoma of the EAC. Early-stage
tumors achieved better local and local-regional control than late-stage
tumors, which translated into a superior cause-specific survival. Less than
half of the patients (13 of 30; 43%) were cured without significant
complications, suggesting a suboptimal therapeutic ratio with our current
approach to local management.
The role of radiotherapy in treating squamous cell
carcinoma of the external auditory canal, especially in early stages of disease.
Hashi N, Radiother Oncol. 2000 Aug;56(2):221-5. .
Department of Radiology, Hokkaido University School of Medicine, North-15 West-7, Kita-ku,
Sapporo, Japan.
The treatment results for 20 patients treated between 1980 and 1998 were retrospectively
analyzed. Radiotherapy was used as an initial treatment without surgery in eight patients
and with surgery in 12 patients. The patients treated by radiotherapy alone received 65 Gy
in 26 fractions over 6.5 weeks. The patients treated with radiotherapy perioperatively
received 30-75 Gy in 12-30 fractions. The follow-up period for survivors including
patients died of intercurrent disease ranged from 7 to 205 months (mean: 71 months).
RESULTS: The 5-year survival rate calculated by the Kaplan-Meier method for all patients
was 59%. According to Stell classification (Laryncol. Otol. 99 (1985) 847), the 5-year survival rates for eight patients with T1 disease and eight with T2
disease were 100 and 38%, respectively. In the eight patients with T1 disease,
disease control was 100%. Local control with hearing preservation was achieved in five
patients with T1 disease by radiotherapy alone. No late complications related to
radiotherapy were observed. CONCLUSIONS: A precise diagnosis of the disease in terms of
whether or not it has invaded the bone is important in order to predict the treatment
outcome. Radiotherapy with or without surgery is the
treatment of choice for patients with T1-stage disease. Surgery with radiotherapy is
recommended as standard care for tumors with bony invasion.
Carcinoma of the external auditory canal and middle ear.
Pfreundner L, Int J Radiat Oncol Biol Phys. 1999 Jul 1;44(4):777-88.
Department of Radiation Oncology, University of Wuerzburg, Germany.
PURPOSE: To evaluate therapeutic modalities used at our institutions regarding local
control, disease-free survival and actuarial survival in carcinoma of the external
auditory canal and middle ear, in an attempt to provide guidelines for therapy. METHODS
AND MATERIALS: A series of 27 patients with carcinoma of the external auditory canal and
middle ear treated between 1978 and 1997 in our institutions were analyzed with particular
reference to tumor size and its relation to surrounding tissues, patterns of neck node
involvement, surgical procedures, and radiation techniques employed. Clinical endpoints
were freedom from local failure, overall survival, and disease-free survival. The median
follow-up was 2.7 years (range 0.1-17.9 years). RESULTS: Treatment
by surgery and radiotherapy resulted in an overall 5-year survival rate of 61%. According
to the Pittsburgh classification, the actuarial 5-year survival rate for early disease (T1
and T2 tumors) was 86%, for T3 tumors 50%, and T4 stages 41%. Patients with
tumors limited to the external auditory canal had a 5-year survival rate of 100%, patients
with tumor invasion of the temporal bone 63%, and patients with tumor infiltration beyond
the temporal bone 38%. The rate of freedom from local recurrence was 50% at 5 years.
Unresectability by dural and cerebral infiltration, and treatment factors such as complete
resection or resection with tumor beyond surgical margins are of prognostic relevance. All
patients with dural invasion died within 2.2 years. The actuarial 5-year survival rate of
patients with complete tumor resection was 100%, but 66% in patients with tumor beyond
surgical margins. 192Iridium high-dose-rate (HDR) afterloading brachytherapy based on
three-dimensional computed tomography (3D CT)-treatment planning was an effective tool in
management of local recurrences following surgery and a full course of external beam
radiotherapy. CONCLUSION:
Surgical resection followed by
radiotherapy adapted to stage of disease and grade of resection is the
preferred treatment of cancer of the external auditory canal and middle ear.
For rational surgical treatment and risk adapted radiotherapeutic management of cancer of
the EAC and middle ear, careful pretherapeutic analysis of the type, position, and size of
tumor and its relationship to surrounding tissues and vital structures in this area by CT
and MRI examinations is required to choose treatment strategies for achieving tumor-free
margins by en bloc resections Gacek and Goodman suggest superficial
parotidectomy in all en bloc resections, because tumor arising in the EAC follows the path
of least resistance to the preauricular soft tissue and region of the glenoid fossa of the
temporomandibular joint The preauricular spread via the fissures of Santorini confirmed by
our findings of intraparotideal lymph node involvement and patterns of tumor invasion
forms the rationale for performing parotidectomy along with temporal bone resections, and
in cases of lymph node involvement, for neck dissections In spite of intraoperative
monitoring of margins of resection, we observed tumor invasion beyond surgical margins
following nerves, vessels, and fasciae. As incomplete surgical excision is the major
reason for treatment failure postoperative radiotherapy was advocated for our
patients.
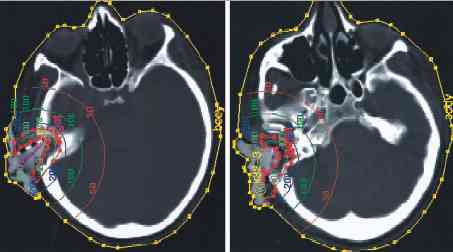
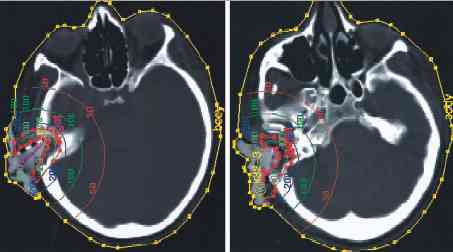
For 3D CT-based EBRT of EAC and middle ear, we established target
volume concepts based on anatomical findings. Rouvi้re describes the
lymphatic capillary network in the EAC continuous with the network of the auricle and the
tympanic membrane. Three zones with different lymphatic drainage are found in the ear
canal: the anterior aspect which drains into the intraglandular and preauricular nodes,
the inferior portion of the canal, which drains inwardly, following the canal to terminate
in deep intraglandular parotideal or infraauricular nodes, and the posterior aspect of the
canal takes a deep course, skirting the origin of the sternomastoid muscle to the nodes
lying there. The capillary network of the tympanic membrane is continuous with that of the
external auditory canal and the mucosal aspect of the middle ear. Thus, we included all possibly involved lymphatic pathways into our target
volume as described above. Since carcinomas of the EAC often invade along the perineural
pathways , dichotomously far beyond macroscopic extension of disease, they become most
difficult to eradicate We take perineural tumor spread into account when defining
target volume. More recently, we integrated the superficial compartment
innervated by the ipsilateral facial nerve into the clinical target volume in these
cases of perineural infiltration of facial nerve. Using this target volume concept, we
achieved local control for a period of 2.4–3.3 years in postoperative situation.
Adenoid cystic carcinomas are a special entity in tumors of the EAC, showing a slow
proliferation rate and a low tendency of lymphatic spread. However, when excised
incompletely, lesions recur locally and the prognosis is poor. We decided for a “wait
and see” policy without postoperative radiotherapy only in completely en bloc
resected patients with adenoid cystic carcinoma and one T1N0 mucoepidermoid
carcinoma when perineural tumor invasion was excluded by histopathological serial
sections. Perzin describes a local recurrence rate of 20% in patients with completely
resected adenoid cystic carcinoma. Shih and Crabtree reported local control in all
patients with completely resected early disease of EAC without postoperative
radiotherapy.
Using external beam radiation based on 3D CT-treatment planning, tumoricidal doses can be
administered without a serious threat of brain stem damage and brain injury.
Postoperative adjuvant radiotherapy with doses of 54–60 Gy
completed treatment of our patients when tumor was resected radically, achieving a local
control and 5-year survival rate of 100%.
The radicality of resection and radiotherapy is a factor influencing local control and
survival. Our patients with tumor beyond surgical margins gained a 5-year survival rate of
66%. In our experience, only a full course of EBRT of more than 66 Gy should be
administered to the tumor bed, as tumor recurred in our series within the planning target
volume in regions which received 66 Gy or less. This may be due to the hypoxia and the
reduced sensibility to radiation of tumor cells at the margin of resection. Many cases of
late stages of cancer of the EAC and middle ear are resected with tumor beyond surgical
margins. This fact, and reduced doses in postoperative radiation treatment, might be the
reason for low local tumor control rates. Shih reported a local control rate for
resected and postoperatively irradiated late stage tumors of the EAC of 45% (5/11) at 2
years, and Wang of 27% (3/11) at 5 years. Extension of the disease beyond the dura
mater is tantamount to unresectability and incurability. Therefore, we believe that
palliative EBRT appears to be the adapted treatment for these patients.
Recurrences after surgery and EBRT exhibit a poor prognosis. Brachytherapy is a treatment
option which can be applied in curative intent when the disease is locally confirmed.
Hammer e reported of HDR intracavitary irradiation of a recurrent transitional cell
carcinoma in the tympanic cavity (11 ื 3 Gy over 4 days, total dose 33 Gy to a spherical
volume, 1.7 cm in diameter) and achieved a disease-free survival of 24 months. The authors
concluded that fractionated HDR brachytherapy can be used to achieve local control in
small volume recurrences at previous irradiated sites. Martinez treated 1 patient having
cancer of the EAC by primary intracavitary HDR-afterloading treatment. The patient
received 6 ื 5 Gy in 6-mm depth calculated from the center of the catheter (1
fraction/week, total dose: 30 Gy). At a 2-year follow-up visit, the patient was free of
tumor and completely asymptomatic. Mayer treated 6 patients after local resection of
tumors of the EAC by LDR and HDR brachytherapy. In 1 patient, 192Iridium HDR brachytherapy
was used for treatment. A dose of 6 ื 5 Gy in 5-mm tissue depth, 1 fraction per week, was
applied. The early disease of EAC cancer was controlled in a follow-up of 2 years. For LDR
treatment, 60Co pearls were applied, and doses of 5 ื 10 Gy in 5-mm tissue-depth were
administered on 5 consecutive days. Four patients were free of disease in a 10-year
follow-up. In 2 patients who had tumor invasion of the temporal bone at the time of
diagnosis, local recurrences became evident. Although there are radiobiological advantages
for LDR-techniques, only 1 of our patients was treated in this way by radium application.
HDR was preferred for our patients because there is an advantage of optimizing the dose
distribution in CT-based treatment planning easily by weighting the dwell positions
individually, thus providing the opportunity of covering the target volume and sparing
healthy tissues as far as possible.
Conclusion
The preferred treatment for cancer of the external auditory canal and middle ear is
radical surgery with tumor-free surgical margins and risk adapted postoperative
radiotherapy.
EBRT covering a target volume including
the petrosal bone, the parotid fossa, the retroauricular, upper jugular, and spinal
accessory lymph nodes. In cases of lymph node involvement the middle and lower jugular and
spinal accessory lymph nodes should also be applied with an adjuvant dose of 54–60 Gy
(single dose 2 Gy). In cases of perineural tumor spread along the facial nerve, the
superficial compartment innervated by the facial nerve should be included in the target
volume. In cases of tumor-involved surgical margins, an EBRT boost should be applied to
the tumor bed, up to a total dose of minimal 70 Gy, to gain local control.
We achieved an overall survival rate of 61% and a freedom of local recurrence rate of 50%
at 5 years. Unresectability by dural and cerebral tumor invasion, and treatment factors
such as complete or incomplete resection are of prognostic relevance: all patients with
dural invasion died within 2.2 years. The survival rate of patients with completely
resected tumor was 100%, and of patients with tumor beyond surgical margins 66% at 5
years. As intracranial tumor infiltration is a sign of incurability, patients with these
patterns of tumor spread should be treated by palliative EBRT. 192Iridium brachytherapy
based on 3D CT-treatment planning is an effective tool in management of local recurrences
after surgery and EBRT.
Carcinoma of the middle ear and external auditory canal.
Hahn SS, Kim JA, Goodchild N, Constable WC. Int J Radiat Oncol Biol Phys.
1983 Jul;9(7):1003-7.
Thirty-one patients with malignant tumors of the middle ear and external auditory canal
(EAC) were observed at the University of Virginia Hospital from 1956 through 1980. Of 27
patients with carcinoma, 21 had squamous cell carcinoma, 4 had basal cell carcinoma and 2
had adenoid cystic carcinoma. One Ewing's sarcoma and 3 rhabdomyosarcomas occurred in an
age group of one to 10 years. The 27 patients with carcinoma are reviewed with regard to
clinical presentation, treatment modality, results and complications. The majority (67%)
of patients had a history of chronic ear drainage, 22% had a previous mastoidectomy or
polypectomy and 7% had an associated cholesteatoma. The treatment modalities employed
depended on the extent of disease and the patient's general condition. Eighty percent of patients with carcinoma limited to EAC were alive and
well at 5 years, compared to 43% of patients with involvement of the middle ear.
Fifty-six percent of patients without invasion of the petrous bone were alive at 5 years
compared to only 20% of patients with petrous bone involvement. The data strongly suggest
that survival depends on the extent of disease. The corrected
disease free 5 year survival rates were 14% for patients who had surgery alone and 50% for
those who had surgery and radiotherapy. Of the three patients with advanced
disease who received radiotherapy alone, none survived five years. Surgery or radiotherapy
alone is not sufficient for most of the cases of carcinoma of the middle ear, since these
patients often present with advanced disease.
We
recommend combined therapy, especially postoperative radiotherapy,
except for early lesions that do not involve the mastoid or petrous bone. Other series
suggest radiotherapy would be adequate and more effective than surgery for early lesions.
Surgery will provide the diagnosis, determine the extent of disease, offer adequate
drainage of infected material and relieve most pain before radiation therapy. |