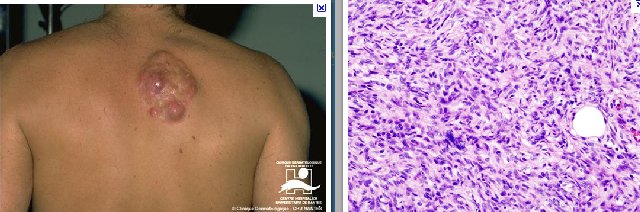
Surgical
resection has long been the
treatment of choice for DFSP
and, ultimately, eradicates the
tumor in a large proportion of
patients. However, DFSP is not
easy to eradicate. The need for
wide excision margins has been
amply documented and is
summarized in. It is generally
recognized that conventional
resection should encompass the
tumor with at least 3 cm of
margin, including underlying
fascia but, even then,
recurrence rates of 10–20% can
be expected . Mohs micrographic
surgical excision has been
associated with low recurrence
rates (<10%) , and may result in
smaller wounds requiring less
complicated repair than
conventional wide excision. The
utility of Mohs surgery might be
further enhanced by
immunohistochemical (anti-CD34)
margin control . The
disadvantage is that this is a
very labor-intensive method that
may be complicated by prior
excision and/or recurrence. Such
meticulous analysis of the
resection margin is particularly
difficult for large masses.
An alternative tissue-conserving strategy for selected patients would be the use of combined conservative resection and radiation. This approach would allow for more limited resection, a strategy that has been successful for other soft tissue sarcomas, including low-grade lesions such as desmoids and atypical lipomatous tumors. Although the number of patients in our series is small, it is among the largest reporting on the combination of surgery and radiation for this disease and supports the conclusion drawn by Suit et al.that, in selected situations, radiation at doses of 50–60 Gy is an effective adjuvant to surgical resection . We observed only one recurrence in 19 patients, 10 of whom had already experienced at least 1 prior recurrence and 6 had positive margins, both recognized as adverse factors in surgical series. Likewise, Suitreported only 3 local recurrences in 15 patients, 5 of whom had a history of prior relapse and 12 had positive margins. Taken together, our data and those of Suit et al. reveal only 4 recurrences among 34 patients (12%), 18 of whom had positive margins. Suit et al. also reported that gross disease was permanently controlled in 3 patients receiving 67–75 Gy (19). Thus, DFSP is a radioresponsive tumor.
Although surgery remains the treatment of choice for DFSP, radiation in doses of 50–60 Gy should be considered as an adjuvant to resection if margins are close or positive. Likewise, if the lesion has already recurred despite wide excision, then reresection with adjuvant radiation may offer the best prospect for eradicating the disease. Furthermore, if obtaining wide resection margins would entail significant cosmetic or functional deficit, consideration should be given to lesser resection that minimally encompasses gross disease, with radiation planned to follow. Finally, for lesions unresectable or resectable only by formidable surgery, the use of radiation alone, as suggested by Suit et al.], should be considered
|
|
|
|