| Metastatic spine tumors affect
a large number of patients each year, resulting in significant
pain,destruction of the spinal column causing mechanical instability, and
neurologic deficits. Standard therapeutic options include surgery and
fractionated external beam radiotherapy. The first option can be associated
with significant morbidity and limited local tumor control. Conversely,
radiotherapy may provide less than optimal pain relief and tumor control,
because the total dose is limited by the tolerance of adjacent tissues, such
as the spinal cord.
The emerging technique of
spinal radiosurgery represents a logical extension of the current
state-of-the-art radiation therapy. It has the potential to significantly
improve local control of cancer of the spine, which could translate into
more effective palliation and potentially longer survival. Spinal
radiosurgery might offer improved pain control and a longer duration of pain
control by giving larger radiobiologic doses.This technique also allows for
the treatment of lesions previously irradiated using external beam
radiation. Another advantage to the patient is
that irradiation can be completed in a single day rather than several weeks, which is not
inconsequential for patients with a limited life expectancy.In addition, cancer patients
may have difficulty with access to a radiation treatment facility for prolonged daily
fractionated therapy. This technique allows for the treatment of lesions previously
irradiated using external beam radiation.Finally, the procedure is minimally invasive
compared with open surgical techniques and can be performed in an outpatient setting.
Similar to intracranial radiosurgery, stereo-tactic radiosurgery now has a feasible and
safe delivery system available for the treatment of spinal metastatic lesions. The major
potential benefit of radiosurgical ablation of spinal lesions is a relatively short
treatment time in an outpatient setting combined with potentially better local control of
the tumor with minimal risk of side effects. CyberKnife spinal radiosurgery offers a new
and important alternative therapeutic modality for the treatment of spinal metastases in
medically inoperable patients, previously irradiated sites, and for lesions not amenable
to open surgical techniques or as an adjunct to surgery.Spinal radiosurgery is likely to
become an essential part of any neurosurgical spine center that treats a large number of
patients with spinal metastases.
CyberKnife frameless stereotactic radiosurgery for spinal lesions: clinical experience in
125 cases.
Gerszten PC, Ozhasoglu C, Burton SA, Vogel WJ, Atkins BA, Kalnicki S, Welch WC. Neurosurgery.
2004 Jul;55(1):89-98;
Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh,
Pennsylvania, USA.
OBJECTIVE: The role of stereotactic radiosurgery for the treatment of intracranial lesions
is well established. Its use for the treatment of spinal lesions has been limited by the
availability of effective target-immobilizing devices. Conventional external beam
radiotherapy lacks the precision to allow delivery of large doses of radiation near
radiosensitive structures such as the spinal cord. The CyberKnife (Accuray, Inc.,
Sunnyvale, CA) is an image-guided frameless stereotactic radiosurgery system that allows
for the radiosurgical treatment of spinal lesions. This study evaluated the feasibility
and effectiveness of the treatment of spinal lesions with a single-fraction radiosurgical
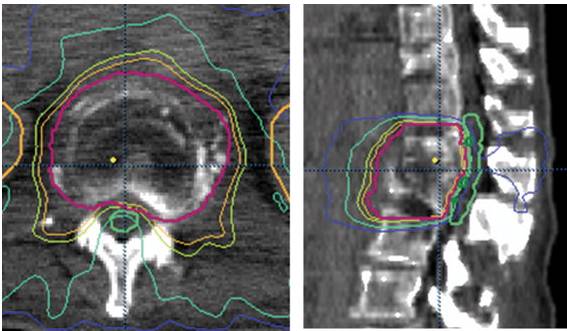
technique using the CyberKnife. METHODS: The CyberKnife system uses the coupling of an
orthogonal pair of x-ray cameras to a dynamically manipulated robot-mounted linear
accelerator with six degrees of freedom that guides the therapy beam to the intended
target without the use of frame-based fixation. Real-time imaging allows the tracking of
patient movement. Cervical spine lesions were located and tracked relative to cranial bony
landmarks; lower spinal lesions were tracked relative to fiducial bone markers. In this
prospective cohort evaluation of a spine radiosurgery technique, 125 spinal lesions in
115 consecutive patients were treated with a single-fraction radiosurgery technique
(45 cervical, 30 thoracic, 36 lumbar, and 14 sacral). There were 17 benign tumors and 108
metastatic lesions. All dose plans were calculated on the basis of computed tomographic
images acquired from 1.25-mm slices with an inverse treatment planning technique.
Radiosurgical circular cones ranging in diameter from 5 to 40 mm were used. RESULTS: Tumor
volume ranged from 0.3 to 232 cm(3) (mean, 27.8 cm(3)). Seventy-eight lesions had received
external beam irradiation previously. Tumor dose was maintained at 12 to 20 Gy to the
80% isodose line (mean, 14 Gy); canal volume receiving more than 8 Gy ranged from 0.0
to 1.7 cm(3) (mean, 0.2 cm(3)). No acute radiation toxicity or new neurological
deficits occurred during the follow-up period (range, 9-30 mo; median, 18 mo). Axial
and radicular pain improved in 74 of 79 patients who were symptomatic before
treatment. CONCLUSION: This is the first large prospective evaluation of this frameless
image-guided spinal radiosurgery system. The CyberKnife system was found to be feasible,
safe, and effective. The major potential benefits of radiosurgical ablation of spinal
lesions are short treatment time in an outpatient setting with rapid recovery and
symptomatic response. This technique offers a successful therapeutic modality for the
treatment of a variety of spinal lesions as a primary treatment or for lesions not
amenable to open surgical techniques, in medically inoperable patients, in lesions located
in previously irradiated sites, or as an adjunct to surgery.
Feasibility of frameless single-fraction stereotactic
radiosurgery for spinal lesions.
Gerszten PC, Ozhasoglu C, Burton SA, Kalnicki S, Welch WC. Neurosurg Focus. 2002 Oct
15;13(4):e2.
Department of Neurological Surgery, University of Pittsburgh School of Medicine, UPMC
Health System, Pittsburgh, Pennsylvania, USA. gerszten@neuronet.pitt.edu
OBJECT: The role of stereotactic radiosurgery for the treatment of intracranial lesions is
well established. Its use for the treatment of spinal lesions has been limited by the
availability of effective target-immobilizing devices. In this study the authors evaluated
the CyberKnife Real-Time Image-Guided Radiosurgery System for spinal lesion treatment
involving a single-fraction radiosurgical technique. METHODS: This frameless image-guided
radiosurgery system uses the coupling of an orthogonal pair of x-ray cameras to a
dynamically manipulated robot-mounted linear accelerator possessing six degrees of
freedom, which guides the therapy beam to the target without the use of frame-based
fixation. Cervical lesions were located and tracked relative to osseous skull landmarks;
lower spinal lesions were tracked relative to percutaneously placed gold fiducial bone
markers. Fifty-six spinal lesions in 46 consecutive patients were treated using
single-fraction radiosurgery (26 cervical, 15 thoracic, and 11 lumbar, and four sacral).
There were 11 benign and 45 metastatic lesions. Tumor volume ranged from 0.3 to 168 ml
(mean 26.7 ml). Thirty-one lesions had previously received external-beam radiotherapy with
maximum spinal cord doses. Dose plans were calculated based on computerized tomography
scans acquired using 1.25-mm slices. Tumor dose was maintained at 12 to 18 Gy to the
80% isodose line; spinal cord lesions receiving greater than 8 Gy ranged from 0 to 1.3
ml (mean 0.3 ml). All patients tolerated the procedure in an outpatient setting. No acute
radiation-induced toxicity or new neurological deficits occurred during the follow-up
period. Axial and radicular pain improved in all patients who were symptomatic prior to
treatment. CONCLUSIONS: Spinal stereotactic radiosurgery involving a frameless
image-guided system was found to be feasible and safe. The major potential benefits of
radiosurgical ablation of spinal lesions are short treatment time in an outpatient setting
with rapid recovery and symptomatic response. This procedure offers a successful
alternative therapeutic modality for the treatment of a variety of spinal lesions not
amenable to open surgical techniques; the intervention can be performed in medically
untreatable patients, lesions located in previously irradiated sites, or as an adjunct to
surgery.
CyberKnife frameless single-fraction
stereotactic radiosurgery for benign tumors of the spine.
Gerszten PC, Ozhasoglu C, Burton SA, Vogel WJ, Atkins BA, Kalnicki S, Welch WC. Neurosurg Focus. 2003 May
15;14(5):e16.
Department of Neurological Surgery, University of Pittsburgh School of Medicine, UPMC
Health System, Pittsburgh, Pennsylvania, USA. gerszten@neuronet.pitt.edu
OBJECT: The role of stereotactic radiosurgery in the treatment of benign intracranial
lesions is well established. Its role in the treatment of benign spinal lesions is more
limited. Benign spinal lesions should be amenable to radiosurgical treatment similar to
their intracranial counterparts. In this study the authors evaluated the effectiveness of
the CyberKnife for benign spinal lesions involving a single-fraction radiosurgical
technique. METHODS: The CyberKnife is a frameless radiosurgery system in which an
orthogonal pair of x-ray cameras is coupled to a dynamically manipulated robot-mounted
linear accelerator possessing six degrees of freedom, whereby the therapy beam is guided
to the intended target without the use of frame-based fixation. Cervical spine lesions
were located and tracked relative to skull osseous landmarks; lower spinal lesions were
tracked relative to percutaneously placed fiducial bone markers. Fifteen patients
underwent single-fraction radiosurgery (12 cervical, one thoracic, and two lumbar).
Histological types included neurofibroma (five cases), paraganglioma (three cases),
schwannoma (two cases), meningioma (two cases), spinal chordoma (two cases), and
hemangioma (one case). Radiation dose plans were calculated based on computerized
tomography scans acquired using 1.25-mm slices. Planning treatment volume was defined as
the radiographic tumor volume with no margin. The tumor dose was maintained at 12 to 20
Gy to the 80% isodose line (mean 16 Gy). Tumor volume ranged from 0.3 to 29.3 ml (mean
6.4 ml). Spinal canal volume receiving more than 8 Gy ranged from 0.0 to 0.9 ml (mean 0.2
ml). All patients tolerated the procedure in an outpatient setting. No acute
radiation-induced toxicity or new neurological deficits occurred during the follow-up
period. Pain improved in all patients who were symptomatic prior to treatment. No tumor
progression has been documented on follow-up imaging (mean 12 months). CONCLUSIONS: Spinal
stereotactic radiosurgery was found to be feasible, safe, and effective for the treatment
of benign spinal lesions. Its major potential benefits are the relatively short treatment
time in an outpatient setting and the minimal risk of side effects. This new technique
offers an alternative therapeutic modality for the treatment of a variety of benign spinal
neoplasms in cases in which surgery cannot be performed, in cases with previously
irradiated sites, and in cases involving lesions not amenable to open surgical techniques
or as an adjunct to surgery.
CyberKnife frameless single-fraction
stereotactic radiosurgery for tumors of the sacrum.
Gerszten PC, Ozhasoglu C, Burton SA, Welch WC, Vogel WJ, Atkins BA, Kalnicki S. Neurosurg Focus. 2003 Aug
15;15(2):E7.
Department of Neurological Surgery, University of Pittsburgh School of Medicine,
University of Pittsburgh Medical Center Health System, Pittsburgh, Pennsylvania, USA.
gersztenpc@msx.upmmc.edu
OBJECT: The role of stereotactic radiosurgery for the treatment of intracranial lesions is
well established. The experience with radiosurgery for the treatment of spinal and sacral
lesions is more limited. Sacral lesions should be amenable to radiosurgical treatment
similar to that used for their intracranial counterparts. The authors evaluated a single-
fraction radiosurgical technique performed using the CyberKnife Real-Time Image-Guided
Radiosurgery System for the treatment of the sacral lesion. METHODS: The CyberKnife is a
frameless radiosurgery system based on the coupling of an orthogonal pair of x-ray cameras
to a dynamically manipulated robot-mounted linear accelerator possessing six degrees of
freedom, which guides the therapy beam to the intended target without the need for
frame-based fixation. All sacral lesions were located and tracked for radiation delivery
relative to fiducial bone markers placed percutaneously. Eighteen patients were treated
with single-fraction radiosurgery. Tumor histology included one benign and 17 malignant
tumors. Dose plans were calculated based on computerized tomography scans acquired using
1.25-mm slices. Planning treatment volume was defined as the radiographically documented
tumor volume with no margin. Tumor dose was maintained at 12 to 20 Gy to the 80%
isodose line (mean 15 Gy). Tumor volume ranged from 23.6 to 187.4 ml (mean 90 ml). The
volume of the cauda equina receiving greater than 8 Gy ranged from 0 to 1 ml (mean 0.1
ml). All patients underwent the procedure in an outpatient setting. No acute radiation
toxicity or new neurological deficits occurred during the mean follow-up period of 6
months. Pain improved in all 13 patients who were symptomatic prior to treatment.
No tumor progression has been documented on follow-up imaging. CONCLUSIONS: Stereotactic
radiosurgery was found to be feasible, safe, and effective for the treatment of both
benign and malignant sacral lesions. The major potential benefits of radiosurgical
ablation of sacral lesions are relatively short treatment time in an outpatient setting
and minimal or no side effects. This new technique offers a new and important therapeutic
modality for the primary treatment of a variety of sacral tumors or for lesions not
amenable to open surgical techniques.
Image-guided hypo-fractionated stereotactic
radiosurgery to spinal lesions.
Ryu SI, Chang SD, Kim DH, Murphy MJ, Le QT, Martin DP, Adler JR Jr. Neurosurgery.
2001 Oct;49(4):838-46.
Department of Neurosurgery, Stanford University Medical Center, 300 Pasteur Drive,
Stanford, CA 94304, USA. seoulman@stanford.edu
OBJECTIVE: This article demonstrates the technical feasibility of noninvasive treatment of
unresectable spinal vascular malformations and primary and metastatic spinal tumors by use
of image-guided frameless stereotactic radiosurgery. METHODS: Stereotactic radiosurgery
delivers a high dose of radiation to a tumor volume or vascular malformation in a limited
number of fractions and minimizes the dose to adjacent normal structures. Frameless
image-guided radiosurgery was developed by coupling an orthogonal pair of x-ray cameras to
a dynamically manipulated robot-mounted linear accelerator that guides the therapy beam to
treatment sites within the spine or spinal cord, in an outpatient setting, and without the
use of frame-based fixation. The system relies on skeletal landmarks or implanted fiducial
markers to locate treatment targets. Sixteen patients with spinal lesions
(hemangioblastomas, vascular malformations, metastatic carcinomas, schwannomas, a
meningioma, and a chordoma) were treated with total treatment doses of 1100 to 2500 cGy
in one to five fractions by use of image-guided frameless radiosurgery with the
CyberKnife system (Accuray, Inc., Sunnyvale, CA). Thirteen radiosurgery plans were
analyzed for compliance with conventional radiation therapy. RESULTS: Tests demonstrated
alignment of the treatment dose with the target volume within +/-1 mm by use of spine
fiducials and the CyberKnife treatment planning system. Tumor patients with at least 6
months of follow-up have demonstrated no progression of disease. Radiographic
follow-up is pending for the remaining patients. To date, no patients have experienced
complications as a result of the procedure. CONCLUSION: This experience demonstrates
the feasibility of image-guided robotic radiosurgery for previously untreatable spinal
lesions. |