Carcinoid Tumors
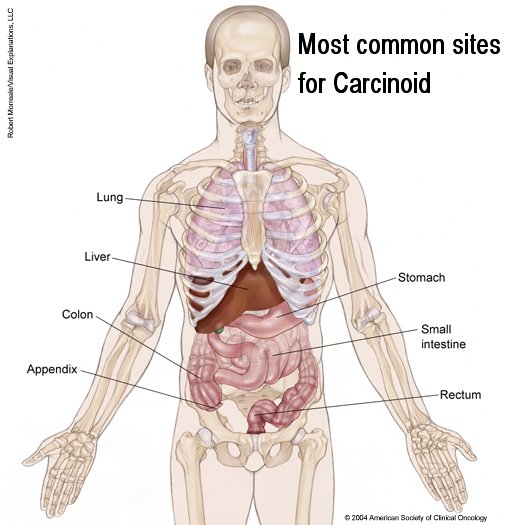 |
A carcinoid
tumor starts in the hormone-producing cells of various
organs, primarily the gastrointestinal tract (such as the stomach
and intestines) and lungs, but also the pancreas, testicles (in
males) or ovaries (in females). A carcinoid tumor is classified as a
neuroendocrine tumor, which means it starts in cells of the
neuroendocrine system that produce hormones.
Here is a general overview of where carcinoid
tumors begin: Some good sites for information about carcinoid: see NCI site, read the ASCO site, go to NCCN and read neuroendocrine tumors, here, here, here, here, and see site on radiation for carcinoids. |
About 85 percent of carcinoid tumors develop in the gastrointestinal tract, usually the appendix. In one report, 44 percent of carcinoids were appendiceal, accounting for more than three fourths of all tumors in that organ.In the same series, the intestine (19 percent), rectum (15 percent), and lung (10 percent) were also frequent sites. Carcinoids account for one third of tumors in the small intestine. Carcinoids of the appendix are commonly incidental findings. The majority are smaller than 1.0 cm and are cured by surgical resection. In the Mayo Clinic series, no tumor of 1.0 cm or less recurred after resection. Therefore, appendectomy alone is adequate treatment. With the uncommon large appendiceal carcinoid, a true cancer operation (e.g., right hemicolectomy) can be required. Carcinoids of the rectum are similar to appendiceal carcinoids and are typically small and are best treated with conservative local measures.
Carcinoids of the small intestine are the most clinically important tumors because of their frequency of presentation, their more advanced stage at diagnosis, and their association with the carcinoid syndrome. The largest and most carefully followed series of patients with small bowel carcinoid has been reported from the Mayo Clinic,where 183 consecutive cases have been followed for a median period of 15 years. Approximately 40 percent of the tumors occurred within 2 feet of the ileocecal valve, with very few in the proximal small intestine. Thirty-five percent of patients had more than one lesion, and most primary tumors were 2.0 to 4.0 cm in diameter. More than 80 percent of patients with resectable primary tumors were free of disease at 20 years. Overall survival in these patients was similar to that of an age- and sex-matched control group. Of the 72 patients who had resected regional node metastases, one half experienced recurrence by 16 years, with continued evidence of relapse after that time. Patients who had unresectable abdominal metastases and hepatic metastases fared least well, with median survival rates of 5 and 3 years, respectively. These data confirm that, even with advanced disease, carcinoid tumors tend to have a relatively indolent course.
Carcinoid Syndrome
Many patients with metastatic carcinoid tumor will manifest the signs and symptoms of abnormal hormone production--the malignant carcinoid syndrome. Serotonin (5-hydroxytryptamine [5-HT]), synthesized by the tumor from tryptophan and metabolized to 5-HIAA, which appears in the urine, is particularly important because urinary 5-HIAA levels are used to monitor the course of carcinoid syndrome. However, the relationship of serotonin levels to symptoms of the clinical carcinoid syndrome is uncertain. Carcinoid tumors also release the enzyme kallikrein,which acts on alpha2 -globulin to produce bradykinin and its precursor, lysyl-bradykinin, both of which can induce flushing. Serotonin may be responsible for intestinal hypermotility and hypersecretion, but it probably does not cause the characteristic flushing that occurs with the carcinoid syndrome. Vasodilation, which causes flushing, can be due to one or more substances released by the tumor cells, including bradykinin, tachykinins, and prostaglandins. The symptoms of the carcinoid syndrome vary in frequency. Flushing is most frequent, followed by diarrhea, heart disease, and bronchoconstriction.
Flushing.
Two types of flushing accompany the usual metastatic ileal carcinoid. One is red and diffuse, involving the face and upper body; it is of short duration and can be provoked by alcohol, excitement, emotional stress, and catecholamine release. The other is more prolonged, produces venous dilation and a purplish hue, and can give rise to permanent dilation of facial veins and telangiectasia. This flush is more commonly precipitated by alcohol ingestion. Since infusion of serotonin does not cause either flush, it has been suggested that the kinins cause this symptom. Brief flushes may be due to catecholamine-induced release of kallikrein; these flushes can be blocked effectively by alpha-adrenergic blocking agents. Carcinoid of the foregut produces a more intense and erythematous flush, sometimes associated with itching, conjunctival suffusion, and facial edema suggestive of histamine.Occasionally, gastric carcinoids cause an urticarial reaction, which may be inhibited by the histamine H1 - and H2 -receptor antagonists diphenhydramine and cimetidine.
Diarrhea.
The diarrhea of carcinoid syndrome does not necessarily correlate with flushing. Diarrhea appears to be related to increased gut motility, rather than to secretion of fluids. Methysergide, a serotonin antagonist, is sometimes effective in treating or preventing diarrhea, hence the presumption that serotonin is directly responsible for this symptom. Infusion of serotonin produces intestinal dysmotility similar to that seen in the carcinoid syndrome.Diarrhea of the carcinoid syndrome is rarely of high volume and, therefore, typically requires only mild palliative antidiarrheal therapy. Although abdominal cramping can be associated with this diarrhea, other possibilities for abdominal pain must be considered, including intermittent partial small bowel obstruction secondary to mesenteric fibrosis or bowel obstruction secondary to tumor bulk.
Heart disease.
The cardiac disease associated with the carcinoid syndrome is an endomyocardial fibrosis typically involving the right side of the heart, although left-sided lesions have been described. Fibrotic deformation of the tricuspid and pulmonary valves usually leads to pulmonary stenosis and tricuspid insufficiency.] In the Mayo Clinic series, carcinoid heart disease was a late complication, with only 5 of 91 deaths identified as having a primary cardiac cause. In that series, most patients with heart disease had high levels of 5-HIAA as well as a lengthy history of carcinoid cardiac disease averaging more than 5 years.Other, relatively rarer, signs and symptoms are associated with carcinoid syndrome. Bronchoconstriction may occur in both pulmonary and extrapulmonary carcinoid and is usually associated with flushing. The classic triad of dermatitis, dementia, and diarrhea seen with pellagra has occasionally been identified. This syndrome is secondary to niacin deficiency as a result of shunting of dietary tryptophan from niacin synthesis to indole synthesis. This is rare, due to better overall nutrition in the population. It is treated with nicotinamide.
The diagnosis of carcinoid tumor is by finding tumor or symptoms related to tumor bulk, biologically active peptides, or from urinary tumor markers. Measurement of 5-HIAA is the most common and reproducible test for the presence of carcinoid syndrome. In most laboratories, the upper limit of normal for 24-hour urinary 5-HIAA excretion is 6 to 10 mg. In one study, 5-HIAA measurements were 100 percent specific and 73 percent sensitive for the presence of carcinoid syndrome. Not all patients with carcinoma tumor have the associated syndrome and the sensitivity of assays for detecting the presence of tumor alone is inadequate. Although markedly elevated 5-HIAA in the urine is remarkably specific for carcinoid tumor, a low-level false-positive increase of 5-HIAA may be seen in patients with noncarcinoid tumor and after intake of certain foods (e.g., bananas, walnuts, and pecans) and medications (e.g., acetaminophen, salicylate, guaifenesin). Also, 5-HIAA may be elevated to low abnormal levels (<30 mg) in patients with diarrhea or malabsorption from any cause. In addition to excellent specificity and high sensitivity, 5-HIAA measurement has a high level of consistency both in individual patients and among groups. In the Mayo Clinic series, the level of 5-HIAA excretion remained constant in a group of 85 patients in whom paired determinations were done during a 10-day period. Moreover, in a given patient, the level of 5-HIAA secretion is a relatively accurate indicator of tumor bulk.] Recently, serum NSE and chromogranin A levels have been shown to correlate with the presence and natural history of gastrointestinal neuroendocrine tumors. Recently, localization of carcinoid and islet cell tumors has been investigated by nuclear medicine techniques, including 123 I-MIBG and octreotide scan
Treatment
Surgery
Nearly one half of all carcinoids arise in the appendix, and most are small and cured by appendectomy.The same is true for small lesions of the rectum, but tumors larger than 2.0 cm in diameter require standard cancer operations. It follows that the surgical approach to bronchial, gastric, or gonadal carcinoid will depend on the location and stage at presentation.Surgery has an important role throughout the course of carcinoid tumor management. Resection of the primary tumor and of associated resectable nodal metastases is primary therapy. Also, complications secondary to recurrent or residual carcinoid may benefit from surgical intervention. These tumors frequently elicit a mesenteric fibrosing reaction, in which the bowel becomes shortened and kinked, frequently causing partial small bowel obstruction. Pain or physiologic abnormalities secondary to partial bowel obstruction may be greatly relieved by palliative surgical resection or bypass, or both. The indolent course of carcinoid tumors mandates a high index of suspicion for such complications and an aggressive approach in considering surgical palliation.
Management of hepatic metastases is important given the frequency of such metastases. In many patients, bulky hepatic metastases constitute most of the tumor burden, so that tumor reduction may, at the least, diminish production of peptides that promote the carcinoid syndrome, as well as extend survival. Principles of surgical management of hepatic metastases are similar to those for islet cell tumors. The indications to proceed with hepatic metastases resection are more liberal in carcinoid tumors than in metastases from other solid tumors. For example, partial resection of hepatic metastases is contraindicated in metastatic colon cancer, as neither effective palliation nor prolongation of survival is achieved. However, the much longer survival in carcinoid tumor makes palliative resection of hepatic metastases appropriate to decrease tumor burden and improve patient well-being. A variety of cancer therapies for hepatic metastases may be attempted, including hepatic irradiation, hepatic embolization, and liver-directed chemotherapeutic agents. These are discussed in the individual treatment sections below.
Radiation Therapy
Radiation therapy is seldomly used to treat carcinoid tumor or carcinoid syndrome. Patients with carcinoid syndrome frequently have extensive hepatic metastases, and the dose-limiting toxicity of hepatic radiation limits its usefulness. Palliative treatment of bone metastases is an indication for radiation therapy. A trial of whole-abdomen radiation therapy (20 to 25 Gy) yielded mixed results, with reduction of abdominal pain but less consistent control of the cancer. Radiation therapy should be considered in patients who require local control and palliation.
Antihormonal Therapy
When the symptoms attributed to serotonin are mild, they can be successfully managed over lengthy periods with simple measures, such as administration of opiates and diphenoxylate hydrochloride with atropine. With more severe symptoms, the peripheral serotonin antagonists methysergide and cyproheptadine are effective in controlling diarrhea and, in some cases, malabsorption. Another approach has been the use of agents known to inhibit serotonin synthesis. alpha-Methyldopa, which partially inhibits the decarboxylation of 5-hydroxytryptophan (5-HTP) to serotonin has been disappointing, except in patients with the rare 5-HTP-secreting metastatic carcinoid of gastric origin.Parachlorophenylalanine (PCPA) inhibits the enzyme tryptophan 5-hydroxylase, which converts tryptophan to 5-HTP, the immediate precursor of serotonin. Although good to excellent control of diarrhea has been observed, the toxic effects of PCPA, including hypersensitivity reactions and mental aberrations, have limited its clinical value.
Somatostatin inhibits carcinoid flush, but is not practical for therapy, since it has a half-life of less than 2 minutes.A synthetic octapeptide analogue of somatostatin has a longer half life, and can be given subcutaneously every 8 to 12 hours to maintain the action of somatostatin. Somatostatin influences the inhibition of numerous gastrointestinal hormones, gastric secretion, gastric and small intestinal motility, splanchnic blood flow, pancreatic enzyme secretion, intestinal nutrient absorption, and gallbladder contractility.Somatostatin analogue has two established uses in carcinoid tumors: chronic treatment of symptomss such as diarrhea and flushing, and treatment of carcinoid crisis. in 1986, described the use of the somatostatin analogue octreotide in therapy for carcinoid syndrome. Fifty-seven patients with carcinoid tumor and carcinoid syndrome were treated with daily doses of octreotide, ranging from 100 to 1,127 mug (mean, 414 mug). Flushing was palliated in most patients, and diarrhea adequately controlled in approximately 75 percent. Control of symptoms was usually associated with a decrease in the urinary 5-HIAA level, but reduction in tumor bulk was not consistently seen. The median duration of response to somatostatin analogue was 4 months, with some patients escaping control quite early, while in others response continued for more than 2 years. Increased doses of somatostatin may partially overcome resistance. More recent studies have confirmed that somatostatin improves symptoms but has little effect on tumor regression.Somatostatin analogue is generally well tolerated.Minimal irritation at the injection site and alterations in bowel patterns have been observed. Fecal fat excretion may also increase, and aberrations in glucose tolerance resulting in hyperglycemia have been observed. Long-term therapy may predispose to the formation of gallstones, since the drug promotes cholelithiasis by inhibition of cholecystokinin release and a resultant inhibition of gallbladder emptying. Approximately 50 percent of patients receiving chronic therapy will develop cholelithiasis and should, therefore, undergo elective cholecystectomy at the time of tumor debulking.
Chemotherapy
Because the disease is indolent there is not much information on the role of chemotherapy. Antineoplastic therapy may be called for in patients whose cancers are aggressive, with progressive liver metastases, signs of partial or impending complete intestinal obstruction, or severe symptoms of carcinoid syndrome uncontrollable by other methods. Controlled clinical trials have been difficult to carry out because of the rarity of the tumor, but cooperative study group trials have been useful in assessing tumor responsiveness. During the 1970s, systemic therapy with single agents was reported, with 5-FU and streptozotocin shown to be active drugs. The Mayo Clinic experience with more than 200 patients suggests that with single agents the response rates of greater than 10 percent was seen with only three adequately tested drugs: doxorubicin, 7 of 33 (21 percent); 5-FU, 5 of 19 (26 percent); and DTIC (dacarbazine) 2 of 15 (13 percent).Based on initial observations of patient response to 5-FU and streptozotocin, investigators at the Mayo Clinic studied that regimen and noted an overall response rate of 33 percent in 43 patients.A larger series of patients was reported in a Phase III study by the Eastern Cooperative Oncology Group (ECOG) comparing 5-FU plus streptozotocin to cyclophosphamide plus streptozotocin. Response rates for the two treatment arms were not significantly different (33 percent vs. 26 percent, respectively), nor were there significant differences in overall survival. Assuming the 5-FU plus streptozotocin regimen to be standard, the ECOG subsequently reported their trial of this combination, with streptozotocin given less frequently to decrease toxicity, compared with doxorubicin alone.Twenty-three percent of patients in each arm responded, further documenting doxorubicin activity.Most recently, ECOG reported the results of their largest trial of combination chemotherapy. This trial randomly allocated patients with measurable carcinoid tumors to the standard regimen of 5-FU plus streptozotocin (FS) and a new regimen of 5-FU and doxorubicin (FA). Patients who had either renal or heart disease making them ineligible for streptozotocin or Adriamycin-containing therapies were treated with DTIC. Of 208 patients who were eligible and analyzed for response and survival, FA and FS associated with response rates of 13 and 16 percent, respectively, in the randomized group. With DTIC, the response rate was approximately 10 percent, with no significant differences between previously treated and untreated patients. Although the response rates for FA and FS did not differ, there was a trend toward improved survival in the FS group. The median survival of the group was 24 months, compared with 16 months for patient receiving FA ( P = 0.11). This suggestive disparity between response rate and survival time may reflect the fact that reduction in tumor bulk has little correlation with survival in patients with an indolent disease such as carcinoid tumor. Alternatively, it may be true that survival is a better measure of tumor response, with inadequate determination of response by traditional techniques. Since no highly effective chemotherapy regimen is available it is clear that patients should be carefully selected for use of cytotoxic chemotherapy in metastatic carcinoid tumor and carcinoid syndrome. Less toxic and more effective palliative therapies for carcinoid syndrome should always be used initially, reserving chemotherapy for those patients who are significantly disabled by unresponsive hormonally related symptoms or those with refractory symptoms due to tumor bulk.
Interferon
Early clinical trials from Sweden suggested a role for low-dose human leukocyte interferon.Subsequently, this group reported the results of three consecutive studies using interferon. In the first study, involving 36 patients, an overall response rate of 47 percent was observed. In the second randomized trial, human leukocyte interferon was compared with FS. No response was observed in the 10 patients treated with chemotherapy, but five patients in the interferon-treated group did respond. In the third study, 20 patients were treated with recombinant interferon; an objective response rate of 55 percent was observed, with the bulk of responses symptomatic and/or chemical responses manifested by a decrease in 5-HIAA, rather than by reduction in tumor bulk. objective regression of tumor bulk occurred in only 11 to 20 percent of cases. The Mayo Clinic subsequently reported the results of their Phase II trial of recombinant interferon-alpha (IFN-alpha) in 24 patients with malignant carcinoid syndrome. Twenty percent of patients with measurable tumor experienced objective tumor regression, and 39 percent had a significant reduction in urinary 5-HIAA excretion. Flushing and diarrhea were transiently relieved, with objective responses lasting less than 2 months. The results suggest a limited role for this agent in carcinoid tumor. Clinical trials are currently being developed in which chemotherapy and interferons are being combined, although early results do not suggest additional benefit compared to single modalities.Similarly, combinations of octreotide and IFN-alpha are being investigated to determine whether lower doses of interferon would be effective and whether the tachyphylaxis associated with octreotide could be overcome by the addition of interferon. Patients with carcinoid tumors treated with interferon may develop a wide variety of autoimmune diseases, such as thyroid disease (thyrotoxicosis, hypothyroidism), pernicious anemia, and vasculitis.
Hepatic-Directed Therapy
The results of surgical resection for hepatic metastases and anecdotal reports of hepatic and abdominal radiation in carcinoid tumors have already been described. The Mayo Clinic has investigated the role of hepatic arterial occlusion in metastatic carcinoid and islet cell tumors. Significant improvement in symptoms and reduction in hepatic metastases were noted in 14 patients with carcinoid tumors, but the median length of response was less than 7 months. Mayo investigators have also investigated the role of sequential hepatic arterial occlusion (HAO), followed by systemic chemotherapy with DTIC and doxorubicin alternating with the combination of 5-FU and streptozotocin in carcinoid tumors.With 65 carcinoid cases treated, more than two thirds of all patients demonstrated objective regression with either HAO or HAO plus chemotherapy. The median duration of regression was longer in the groups receiving chemotherapy, but this was not a randomized trial and better-risk cases may have been selected for the chemotherapy plus HAO treatment. Other groups are investigating the role of selective hepatic arteriography with sequential hepatic arterial embolization or chemoembolization. Significant reduction in the signs and symptoms associated with both carcinoid tumors and islet cell tumors have been reported in the majority of patients so treated. In a study of 15 patients with advanced metastatic carcinoid tumors, hepatic artery chemoembolization improves symptoms and short-term quality of life. Unfortunately, there is a paucity of data on the benefit of either intermittent or prolonged continuous hepatic arterial infusion of chemotherapeutic agents in patients with metastatic carcinoid tumors.