|
INTRODUCTION Brain abscess is a focal collection
within the brain parenchyma, which can arise as a complication
of a variety of infections, trauma, or surgery. Bacteria can invade the brain either by
direct spread, which accounts for 20 to 60 percent of cases, or
through hematogenous seeding . Bacteremic spread typically
causes multiple lesions.
Direct spread The direct spread of organisms from a contiguous site usually causes a single brain abscess. Primary infections that can directly spread to the cerebral cortex include :
Hematogenous spread Brain abscesses associated with bacteremia usually result in multiple abscesses that are most commonly located in the distribution of the middle cerebral artery . Abscesses usually form at the grey-white matter junction where micro infarction damages the blood-brain barrier. Primary infections that lead to hematogenous seeding of the brain include :
No primary site or underlying condition can be identified in 20 to 40 percent of patients with brain abscess depending upon the series . The location of a brain abscess reflects the site of the primary infection that spreads to the cerebral cortex. These locations in the brain in order of decreasing frequency are :
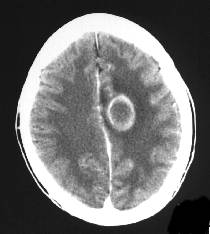
Computed tomographic scan CT scan is not as sensitive as MRI for the diagnosis of brain abscess but can frequently be obtained more easily on an emergent basis. When looking for a brain abscess, this study must be performed with a contrast agent. The lesion has different appearances depending upon its age:
Magnetic resonance imaging MRI should be performed with gadolinium diethylenetriamine peta-acetic acid. This agent increases the T1 intensity and causes more prominent enhancement of lesions than CT scan. Compared to CT scan, MRI:
enhancement, and cerebral edema
Diffusion-weighted MR imaging (DWI) is capable of differentiating ring-enhancing lesions due to brain abscess from neoplastic lesions . Abscesses are usually hyperintense on DWI (indicating restricted diffusion, characteristic of viscous materials, such as pus), while neoplastic lesions are hypointense or show variable hyperintensity that is lower than the intensity seen with an abscess.
|