Douglas Kondziolka, M.D., University of Pittsburgh Medical Center
Approximately 20-40% of patients with systemic malignancies
develop brain metastases. There appears to be a trend toward an increasing incidence of
brain disease, and patients with systemic malignancies can live longer because of earlier
diagnosis and/or better treatment. Many brain tumors are now identified in asymptomatic
patients as part of screening neuroimaging studies. The two most
commonly used treatments, whole-brain radiation therapy (WBRT) and stereotactic
radiosurgery (SR), extend survival from 3 months to 5 months and from 7 months to 13
months, respectively, depending on tumor type.
Surgical resection can be a valuable approach for patients with larger symptomatic tumors.
Although the value of radiosurgery in obtaining local tumor control and extending survival
compared with WBRT alone has been substantiated, the status of long-term survivors and the
reasons for their better outcome remain unclear. Numerous studies have confirmed that the
extent of extracranial disease correlates directly with survival. What remains unclear is
whether successful or unsuccessful care for systemic malignancy, together with aggressive
brain tumor care, can lead to prolonged survival. We are faced with the challenge of
improving survival for patients with brain metastases and managing late complications or
recurrences that previously were unseen as our overall management of cancer improves.
Stereotactic radiosurgery, with or without whole-brain radiation therapy, has become a
valued management choice for patients with brain metastases, although their median
survival remains limited. In patients who receive successful extracranial cancer care,
patients who have controlled intracranial disease are living longer. The authors evaluated
all brain metastasis in patients who lived for 4 years after radiosurgery to determine
clinical and treatment patterns potentially responsible for their outcome.

METHODS
Six hundred seventy-seven patients with brain metastases underwent 781 radiosurgery
procedures between 1988 and 2000. Data from the entire series were reviewed; and, if
patients had 4 years of survival, then they were evaluated for information on brain and
extracranial treatment, symptoms, imaging responses, need for further care, and management
morbidity. These long-term survivors were compared with a cohort who lived for < 3
months after radiosurgery (n = 100 patients).
RESULTS
Forty-four patients (6.5%) survived for > 4 years after
radiosurgery (mean, 69 mos with 16 patients still alive). The mean age at
radiosurgery was 53 years (maximum age, 72 yrs), and the median Karnofsky performance
score (KPS) was 90. The lung (n = 15 patients), breast (n = 9 patients), kidney (n = 7
patients), and skin (melanoma; n = 6 patients) were the most frequent primary sites. Two
or more organ sites outside the brain were involved in 18 patients (41%), the primary
tumor plus lymph nodes were involved in 10 patients (23%), only the primary tumor was
involved in 9 patients (20%), and only brain disease was involved in 7 patients (16%),
indicating that extended survival was possible even in patients with multiorgan disease.
Serial imaging of 133 tumors showed that 99 tumors were smaller (74%), 22 tumors were
unchanged (17%), and 12 tumors were larger (9%). Four patients had a permanent neurologic
deficit after brain tumor management, and six patients underwent a resection after
radiosurgery. Compared with the patients who had limited survival
(< 3 mos), long-term survivors had a higher initial KPS (P = 0.01), fewer brain
metastases (P = 0.04), and less extracranial disease (P < 0.00005).
CONCLUSIONS
Although the expected survival of patients with brain metastases may be limited, selected patients with effective intracranial and extracranial care for
malignant disease can have prolonged, good-quality survival. The extent of extracranial
disease at the time of radiosurgery was predictive of outcome, but this does not
necessarily mean that patients cannot live for years if treatment is effective.
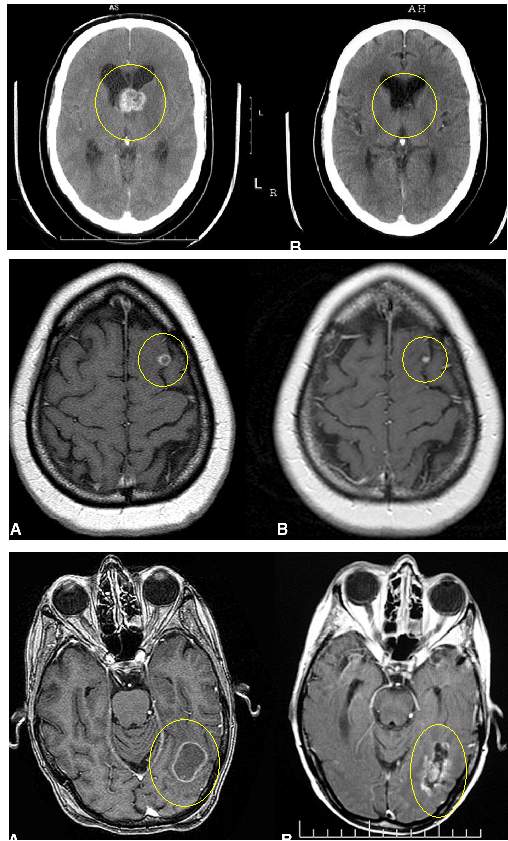
MRI Images of Patients 5 Years after Gamma Knife for Brain Metastases